10 Rhegmatogenous Retinal Detachment – Vitrectomy
10.2 Removal of Non-dissolving Endotamponades (Silicone Oil, Heavy Oil, Heavy Liquids)
Non-gas endotamponades that don’t dissolve (silicone oil, heavy oil, heavy liquids) usually need to be removed to avoid complications such as emulsification or glaucoma (silicone oil) or retinotoxicity (heavy liquids). Usually, vision will also improve following removal of the endotamponade. The exception is when silicone oil is intentionally left in the eye indefinitely due to poor visual prognosis, risk of re-detachment and to prevent phthisis bulbi.
Silicone oil is usually removed several weeks to months following surgery for complicated retinal detachment surgery or advanced proliferative diabetic retinopathy (tractional retinal detachment or recurrent vitreous hemorrhage). The timing of removal should be when the oil has achieved its purpose of stabilizing the retina but before oil-related complications occur. A typical timeframe is between 6 weeks and 6 months. Silicone oil should be removed:
- In most cases after several weeks (6-8 weeks), when the retinal detachment is deemed to be stable. In cases with extensive proliferation or trauma, the time between the initial surgery and the silicone oil removal may be longer as the healing process may take longer and stability is reached later
- If there are signs of emulsification of the silicone oil. This occurs earlier in younger patients, those with trauma, significant hemorrhage, trans-oil laser / cryotherapy, oil underfill and patients with greater post-operative mobility
- If there is silicone oil in the anterior chamber causing secondary band keratopathy
- If there is uncontrolled glaucoma secondary to silicone oil
- If retinal detachment is present beneath the silicone oil (unless it has been decided to leave it in indefinitely)
Prior to removal of silicone oil, retinal optical coherence tomography (OCT) can be performed to investigate for epiretinal membranes that may be difficult to see clinically. These may be peeled at the time of surgery.
With current vitrectomy machines, it is possible to remove most oil easily through a 23- or 25-gauge trocar. The higher the viscosity of the oil, the slower the oil removal and the longer it takes. Larger (e.g. 23-) gauges may be preferred for speed. Oil is usually removed with a VFC system set to extrusion.
1. Remove Oil with a VFC System
- Insert the three valved sclerotomy cannulae and switch the infusion on after visualizing its location in the vitreous cavity
- Raising the intraocular pressure temporarily is useful as oil often refluxes up the infusion line, and the eye will collapse with hypotony if VFC extrusion is performed before adequate infusion has been established. Once the BSS is flowing through the infusion line into the eye, the intraocular pressure can be normalized
- Watch carefully for when the oil has almost been completely removed. It’s is important to reduce the vacuum at this point- once the oil has been removed the eye will collapse as the infusion pressure won’t be sufficient to compensate for the VFC extrusion of BSS. Watch for the meniscus of the oil bubble and try to keep the VFC cannula within the oil at all times. The VFC cannula can be used to tilt the sclerotomy it is entering to the highest point of the eye. This ensures that the tip of the VFC cannula stays in the oil bubble which floats. The VFC cannula can also be used to gently ballotte the eye to monitor the intraocular pressure
- After the VFC has been used to remove as much oil as possible, the eye can be rotated by holding one of the superior cannulae to position this at the highest point of the eye. The valve of the cannula can be opened with forceps to allow for egress of residual oil
Note
- Avoid placing the infusion cannula near the sclerostomy where the oil will be removed. If this occurs there is a tendency to remove the infusing BSS® rather than the silicone oil.
2. Remove Any Silicone Oil From the Anterior Chamber (Figure 10.2.1)
Especially in cases where emulsification has occurred, small oil bubbles may migrate from the posterior segment through the zonular fibres into the anterior chamber. If required, removal of anterior chamber oil is often best performed after removing silicone oil from the vitreous cavity (since more may migrate anteriorly during this procedure), but before vitrectomy (as it will impede visualisation of the fundus).
- Create a paracentesis using 15 degree blade
- Open the paracentesis with .12 forceps to let the oil out passively. Tilt the eye so that the paracentesis is at the highest point of the eye
Alternatively, anterior chamber oil can be removed with:
- Rycroft cannula on a 3ml (cc) syringe filled with BSS® (alternate between injecting BSS® and aspirating oil)
- The vitrector cutter. NB: The vitrector cutter has residual vacuum- it can be turned on then off outside the eye before removing intracameral oil. Aggressive aspiration with the vitrector cutter can lead to collapse of the anterior chamber. To avoid this a bimanual irrigation aspiration system can be setup by moving the infusion cannula to the anterior chamber
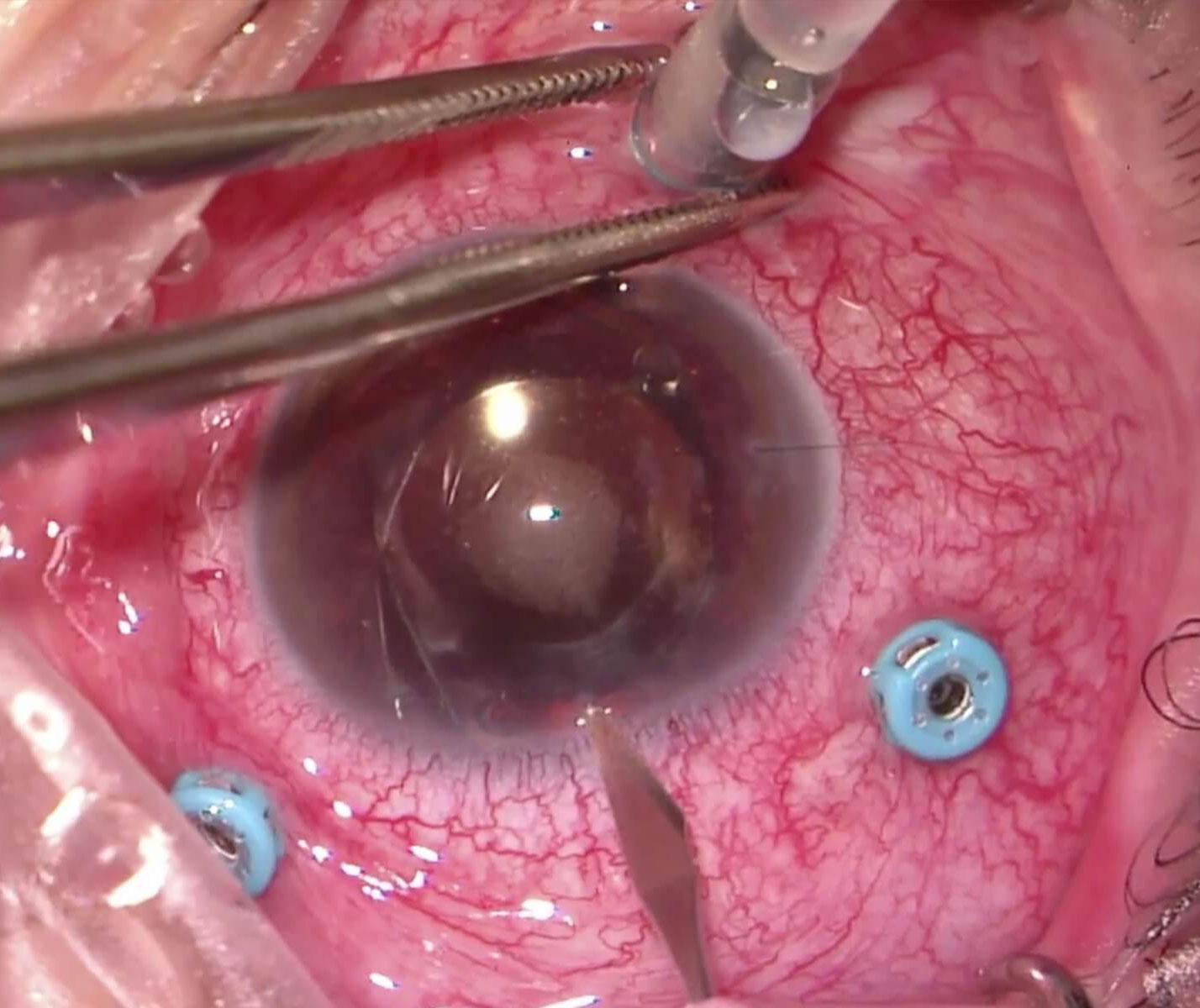
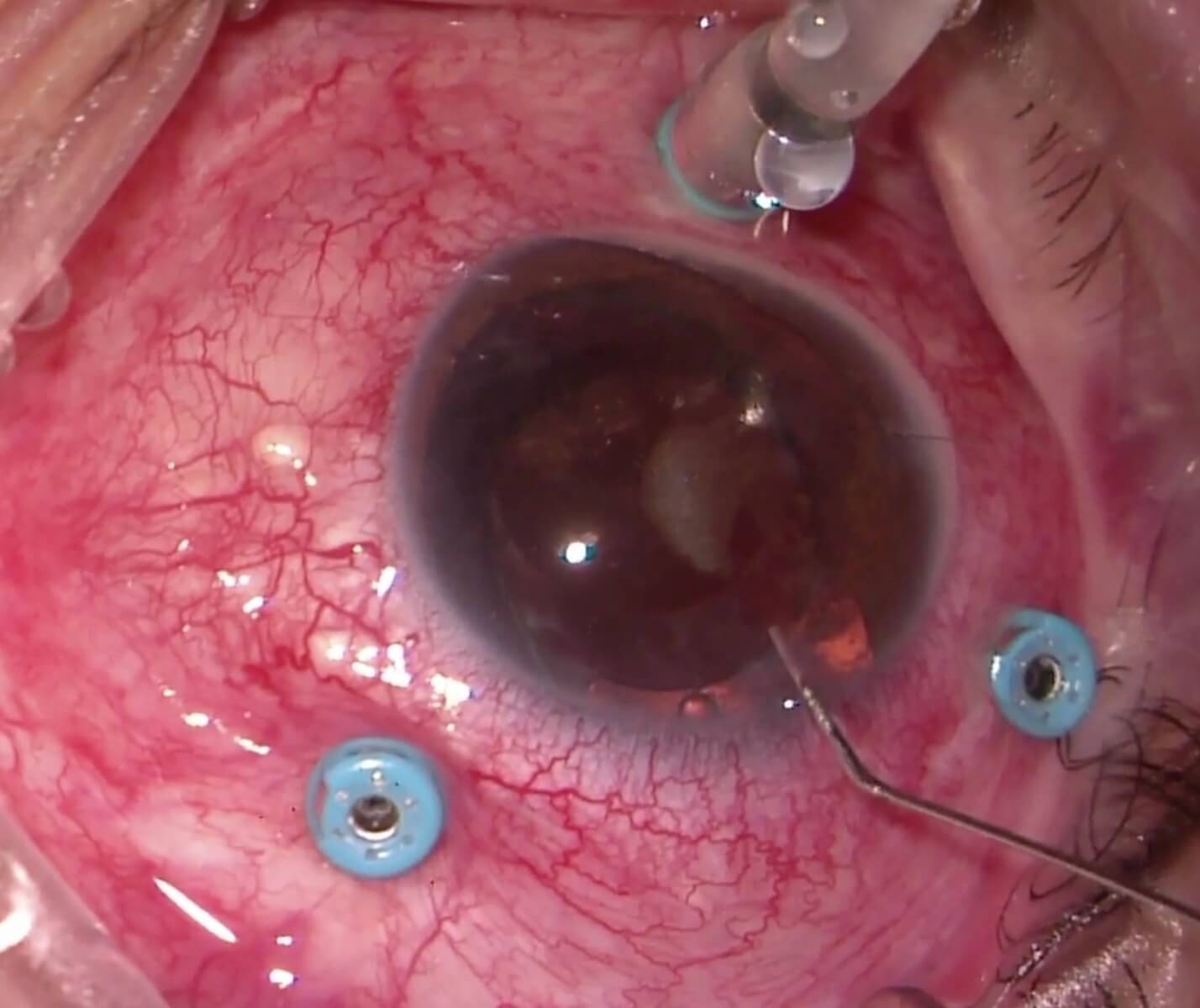
Figure 10.2.1 Removal of Silicone Oil From the Anterior Chamber
A: Paracentesis with a 15 degree blade.
B: Removal of oil through the paracentesis. The paracentesis is opened with .12 forceps and the eye rotated so that the paracentesis is the most superior point. Irrigation is performed with a Rycroft cannula
Figure 10.2.1 Removal of Silicone Oil From the Anterior Chamber
A: Paracentesis with a 15 degree blade.
B: Removal of oil through the paracentesis. The paracentesis is opened with .12 forceps and the eye rotated so that the paracentesis is the most superior point. Irrigation is performed with a Rycroft cannula
3. Vitrectomy to Remove Remaining Oil
Often there is a small amount of residual oil. This can be removed with a vitrectomy cutter or soft-tip extrusion cannula with active extrusion:
- Perform a partial fluid-air exchange, aspirating off the top of the BSS® meniscus (where the oil will be floating) to remove small bubbles of oil (Figure 10.2.2). The greatest yield of oil removal is when most of the BSS has been removed from the eye, but care must be taken not to traumatize the optic disc. A soft-tip extrusion cannula has the advantage of being less traumatic, but the disadvantage of “sticking” oil to its silicone tip
- Switch back to fluid infusion, taking care that the stream of fluid does not damage or re-detach the retina (the stream can be broken by the vitrector cutter)
- Repeat if necessary to remove all the oil
Previous
10.1 Vitrectomy Repair
Next
11.1 Scleral Buckle
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.