3 Vitreoretinal Surgery Fundamentals
3.2 Closure
- Consider reducing the IOP to 15-20mmHg for scleral depression
- Using a scleral depressor, muscle hook or cryotherapy probe) to indent the sclera, check the peripheral retina for iatrogenic tears. Pay particular attention to the trocar entry sites. The peripheral search should be performed prior to FAX, because air decreases the visibility of breaks
- Breaks can be treated with:
i. Laser (In General the Author’s Preference)
- In attached retina, laser can be applied under fluid. This has the advantage of reduced reflections. However, fluid beneath detached retina must be drained before laser. In addition, following fluid air exchange the view of the periphery is improved by the prismatic effect of the vitreous base. This runs the risk of a pseudophakic patient developing fogging of the IOL. This can be addressed by injecting viscoelastic to coat the posterior surface of the IOL, or directing a stream of air from the infusion cannula towards the IOL. In aphakic patients without an intact posterior capsule, air can enter the anterior chamber, impairing visualisation. Consider marking the breaks with endodiathermy before FAX
ii. Cryotherapy
- Cryotherapy can be applied both under fluid and under air. Its advantages over laser include: being able to “highlight” and confirm the presence of small, subtle breaks; easier application through cloudy media and lower cost. However, it is more pro- inflammatory than laser and excessive use may be associated with a higher risk of proliferative vitreoretinopathy (PVR) following retinal detachment surgery. This is yet to be proven
- Small, iatrogenic breaks that occur within the posterior pole (e.g. during membrane peel) and have been relieved of all vitreous traction do not always require application of endolaser so long as an air or gas endotamponade is injected
Perform at least a partial fluid-air exchange (so that the fluid meniscus lies below the sclerostomies). Having air on the inside of the sclerotomies prevents vitreous exiting the wounds, as it tends to stick to the interior of the eye wall, and enhances self-sealing. In addition, it helps to determine if the wounds are air tight - the sclerostomies will “bubble” if not and should be sutured.
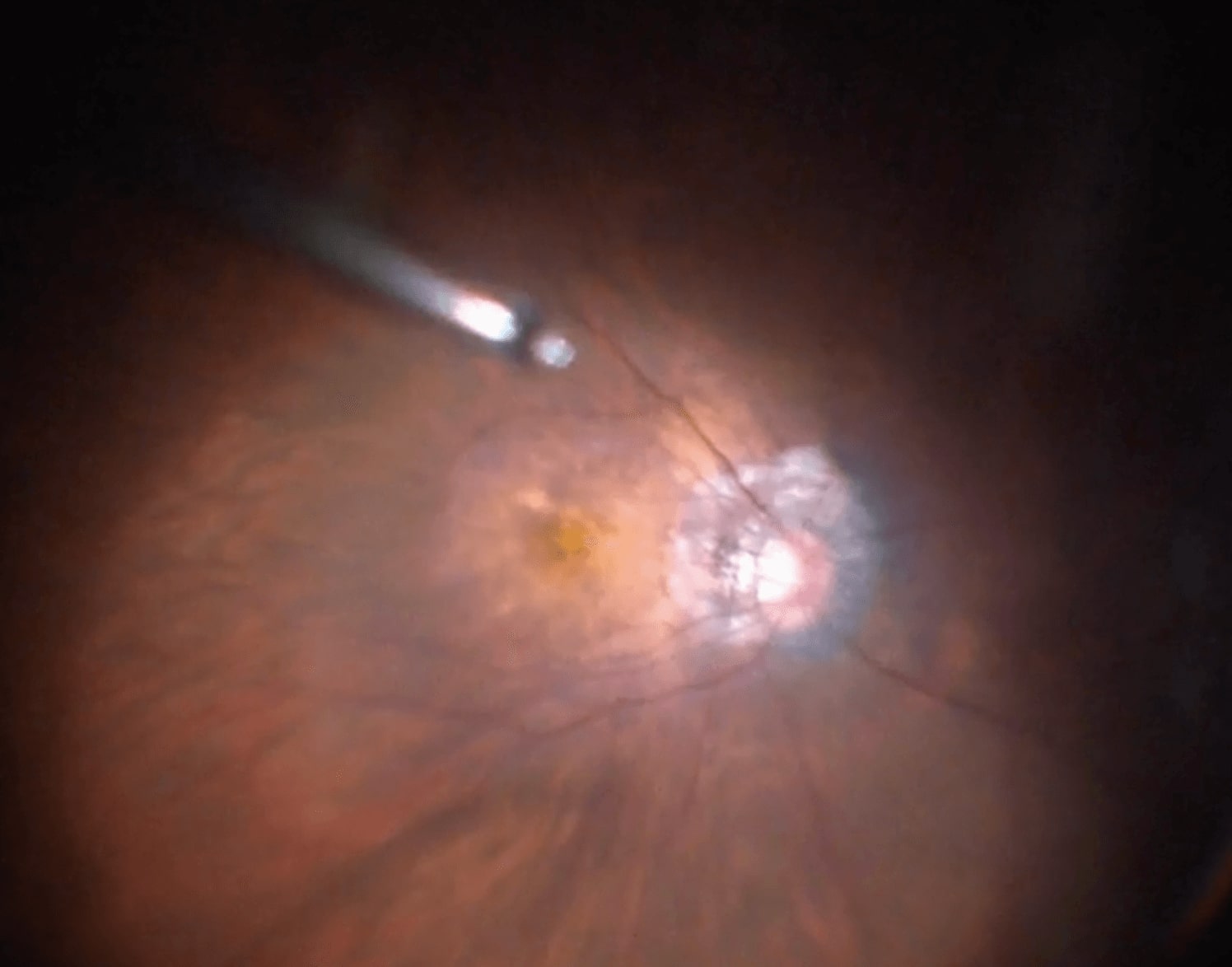
If, during the fluid-air exchange in a phakic patient a “donut” of air develops peripherally (trapped between the lens and vitreous base), insufficient vitrectomy has been performed and more is required (Figure 3.2.1).
A. Small Gauge (23, 25 or 27-gauge)
Remove the superior (light pipe and vitrector) cannulae. Remove the cannula at the same angle that it was inserted. One can insert an instrument such as the light pipe or vitrector cutter into the cannula to plug the port and pull the cannula up around it. This potentially prevents vitreous prolapse into the wound.
Adjust the IOP if necessary before removing the infusion cannula.
Sutureless:
After removing each cannulae, use a cotton bud (q-tip) or tip of the cannula to momentarily press on the anterior lip of the wound. This ensures better closure of the sclerostomy if it is not to be sutured. Some surgeons use the reverse end of a cotton bud (q-tip). Others like to gently “squeeze” the sclerostomies using conjunctival / Moorfields forceps, which facilitates closure.
Suturing Small-gauge Sclerostomies:
Suturing the sclerostomies is necessary under the following circumstances:
- Wound leak (more common if the peripheral vitreous has been removed, larger gauge, longer procedures)
- Silicone oil or heavy liquid (PFO) insertion (subconjunctival oil should be prevented at all costs)
- Situations when hypotony must be avoided – e.g. intraoperative hemorrhage
Most surgeons use 7-0 or 8-0 Vicryl in 3-1-1 throws. Use a blunt forceps to hold one of the other cannulae while suturing. If unsure where the sclerostomies are (e.g. because of conjunctival ballooning), use the back (bent part) of the needle holder to flatten the conjunctiva over the sclerostomy to allow visualization. Some surgeons tie a 4-throw bowtie suture and remove it at the slitlamp on the first post-operative day (not for silicone oil). Subconjunctival gas can be removed using a 30G needle on an empty syringe (it will stay subconjunctival for weeks in case of C3F8).
(C): If a complete fluid-air exchange is required, a silicone soft-tipped extrusion cannula is safer to use than the vitrectomy cutter. Fluid can be drained at the optic disc.
B. 20 Gauge
- Suture the superior (light pipe and vitrector) sclerostomies Suture the superior sclerostomies with cross stitch (“N”) 7-0 vicryl. Use .12 forceps to hold one edge of the sclerostomy
- Suture passes should be just distal to the edges of wound (aim for a square “box stitch”). 3-1-1 throws, cut short
- Suture the infusion sclerostomy
- Adjust the IOP to ~20mmHg before removing the infusion cannula. Pull the short end of the slip knot on the pre-placed suture and remove the suture loops off the cannula
- Pull each end alternately to loosen the proximal side
- Hold the cannula with forceps, then remove the “U” loop off distal end
- Use two needle holders to hold the ends of the suture and lay the suture down flat
- Pull firmly whilst the assistant pulls out infusion line (tell your assistant when you are ready)
- Tie off the suture (1-1 more throws)
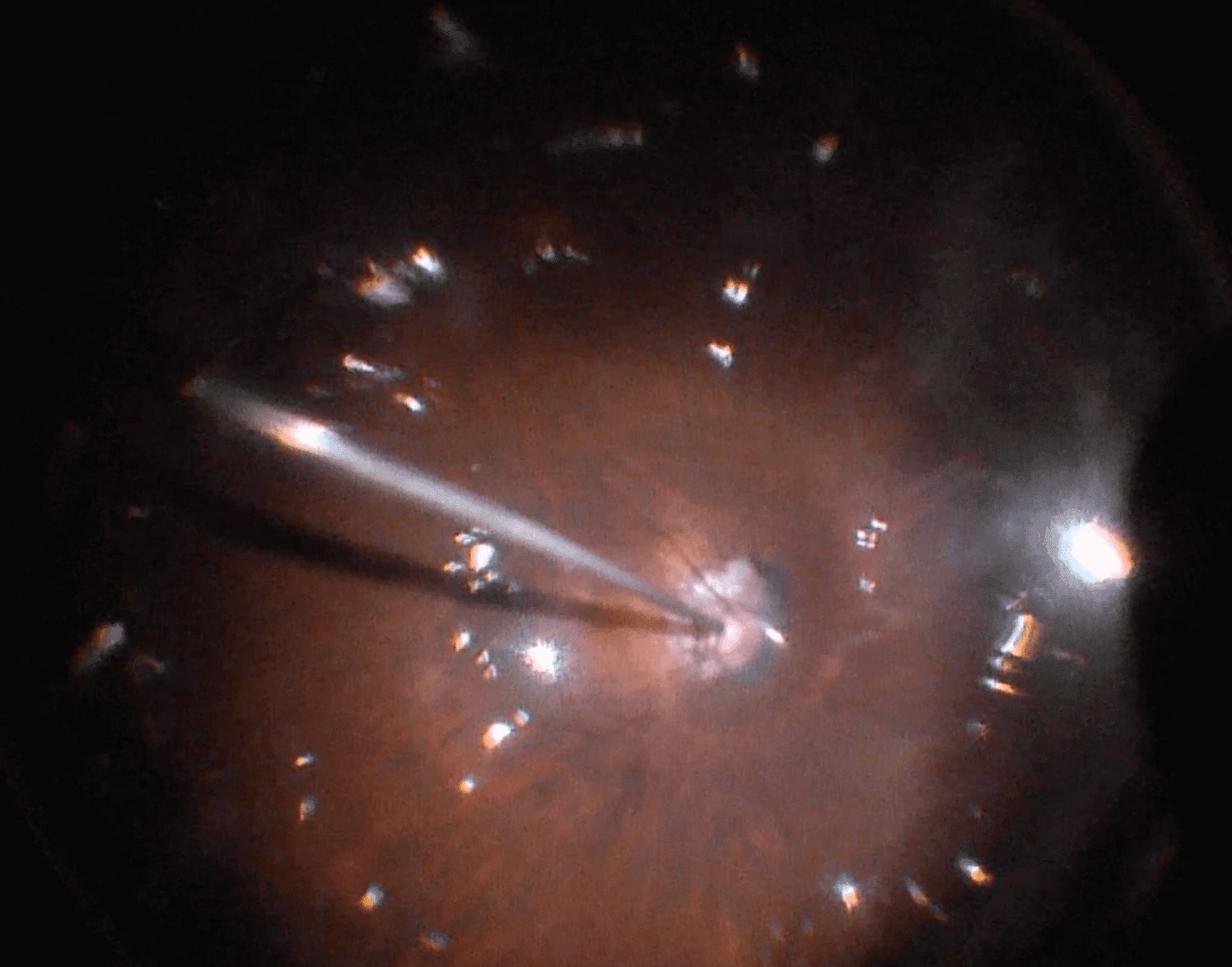
(See Figure 3.2.2)
e.g. Subconjunctival cephalexin and dexamethasone.
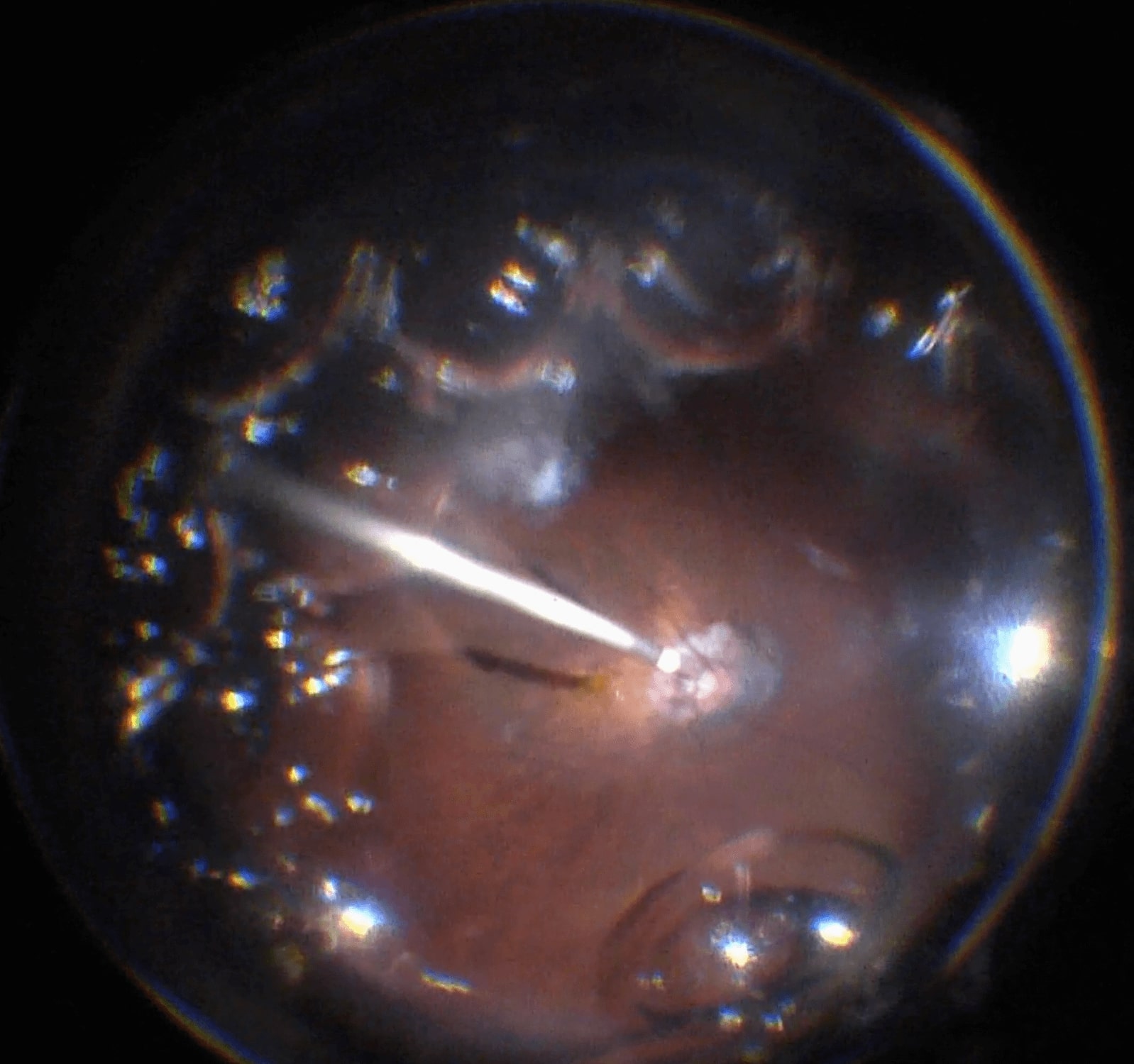
Most surgeons choose to inject subconjunctival antibiotics (e.g. a cephalosporin) and steroid (e.g. dexamethasone) at the conclusion of the operation (Figure 3.2.3). Injecting these near the sclerostomy sites further displaces the conjunctiva from these sites. Warn the patient that they may feel a “sting” prior to injecting. Under certain circumstances (e.g. macular oedema, uveitis), intravitreal or posterior sub-Tenon’s triamcinolone acetonide may be indicated (Figure 3.2.4 and Figure 3.2.5).
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.