18 Symptomatic Vitreous Opacities
18.1 Vitrectomy for Symptomatic Vitreous Opacities
Indications for vitrectomy for symptomatic vitreous opacities include:
- Visually significant idiopathic floaters (associated with vitreous syneresis)
- Visually significant vitreous opacities related to prior ocular inflammation or hemorrhage
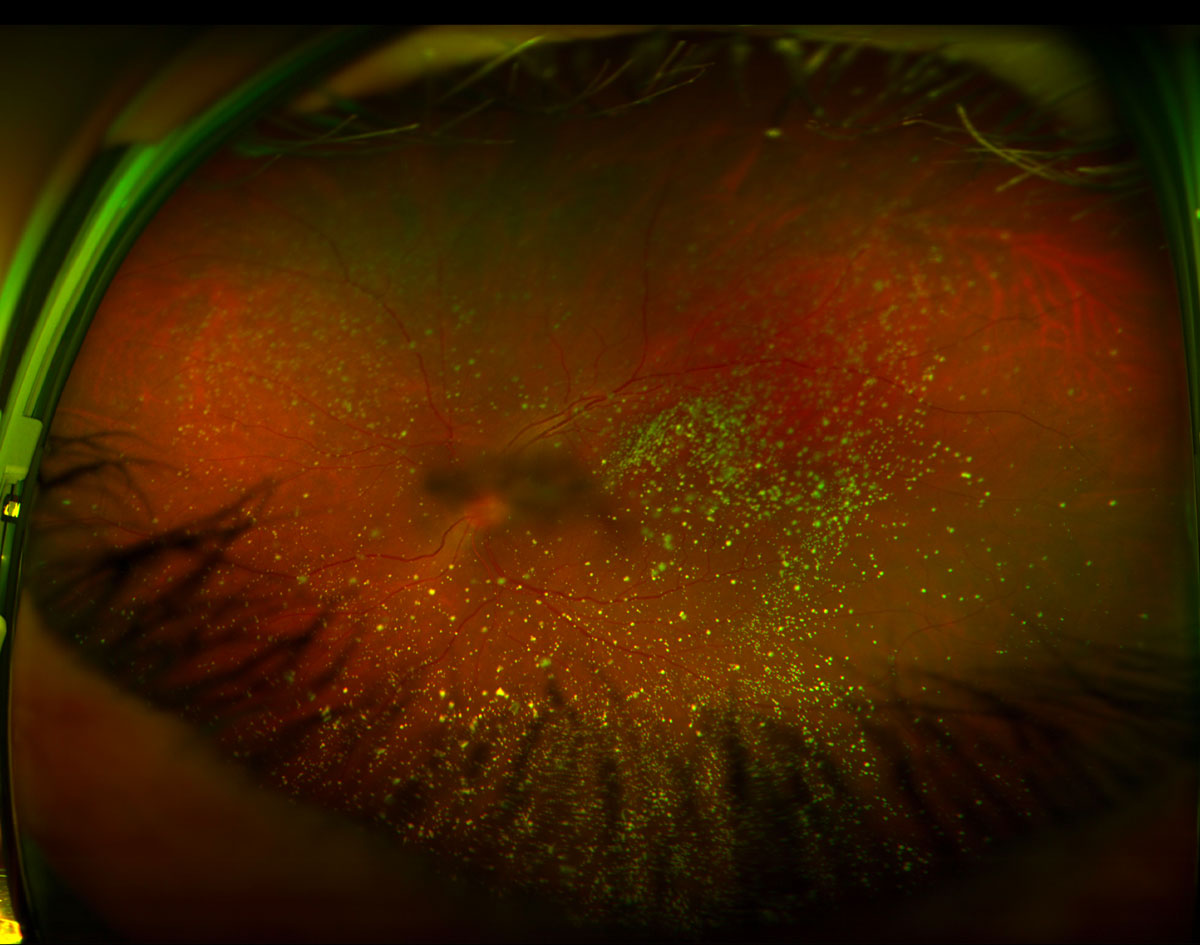
- Vitreous opacities related to symptomatic asteroid hyalosis (Figure 18.1.1)
Vitreous floaters occur commonly. Fortunately, the majority of vitreous floaters do not impact vision enough to affect patient quality of life. However, some individuals experience degradation in contrast sensitivity function and experience vision-degrading myodesopsia. A study by Rostami et al[1] showed that vitrectomy for visually significant floaters improved best corrected visual acuity, contrast sensitivity, and patient quality of life. Furthermore, vitrectomy surgery is highly cost-effective from a health-economics perspective.[1]
It is important to manage expectations when counseling a patient who desires surgery for floaters. Since most patients with visually symptomatic floaters have excellent objectively measured visual acuity, the risks of vitrectomy surgery, including acceleration of cataract, post-operative vitreous hemorrhage, retinal tear and or retinal detachment, and endophthalmitis should be carefully explained to the patient. Often, patients complain of bothersome floaters while performing near tasks or in bright illumination environments in which the contrast for the vitreous opacity is greatest. Such patients with mild symptoms can be persuaded to learn to adapt with tips on better lighting conditions to reduce scattering of incident light by clumps of vitreous opacities. Some patients complain of severe floaters but if the clinical exam fails to confirm their presence, the option for surgery may be discussed. Patients who benefit from vitrectomy generally have significant debris in the vitreous cavity over the posterior pole that move in and out of vision with saccades, rather than a single smudge / floater in their vision. Patients with multifocal lenses may be more symptomatic. Those who find that their activities of daily living (e.g. driving) are impaired by the floaters will benefit the most from surgery.
Vitrectomy for symptomatic floaters is ideally reserved for pseudophakic patients with pre-existing posterior vitreous detachment; however, the patient population primarily presenting with myodesopsia may not match these requirements (Figure 18.1.2). Presence of extensive peripheral pathology or lattice degeneration is a relative contraindication given a higher risk of retinal breaks. A small gauge pars plana vitrectomy set up is preferred to minimize morbidity from the procedure.
Rostami B, Nguyen-Cuu J, Brown G, et al.: Cost-Effectiveness of Limited Vitrectomy for Vision-Degrading Myodesopsia. Am J Ophthalmol 204:1-6, 2019
- Placing ports
- 3 cannulae are placed in standard fashion
- Vitrectomy
- Typically, condensed vitreous opacities over the posterior pole are evident intraoperatively which are the source of patient’s symptomatic floaters, so it is important to perform a complete core vitrectomy by engaging the cutter near the port and travelling around the periphery in an arcuate fashion. If a posterior vitreous detachment (PVD) is not present it is preferable to induce this to achieve full clearance of the vitreous. This decision needs to be balanced with the degree of posterior hyaloid attachment (often inversely proportional to the patient’s age) as elevation of strongly adherent hyaloid is more likely to cause iatrogenic tears. Further details regarding PVD induction can be found in the Chapter 4 PVD Induction. Generally, peripheral shave with scleral depression is not necessary
- Peripheral exam
- Once a complete core vitrectomy is performed, it is important to do a thorough check of the peripheral retina with scleral depression. Retinal tears or areas suspicious for retinal breaks should be treated with laser retinopexy
- Closing
- The ports are removed and leaking sclerostomies closed in standard fashion
Previous
Chapter 17 Endophthalmitis
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.