Chapter 4
4 Posterior Vitreous Detachment Induction
In most vitrectomy operations (retinal detachment, full thickness macular holes etc.), ensuring that a posterior vitreous detachment (PVD) is present is essential. In other cases the need to elevate the posterior hyaloid needs to be balanced against the risk of inducing an iatrogenic retinal tear or detachment. This is more likely to occur if the posterior hyaloid is firmly adherent.
- Clear the sclerostomy sites and perform core vitrectomy
- Switch from the cutting to the aspiration mode of the vitrectomy cutter
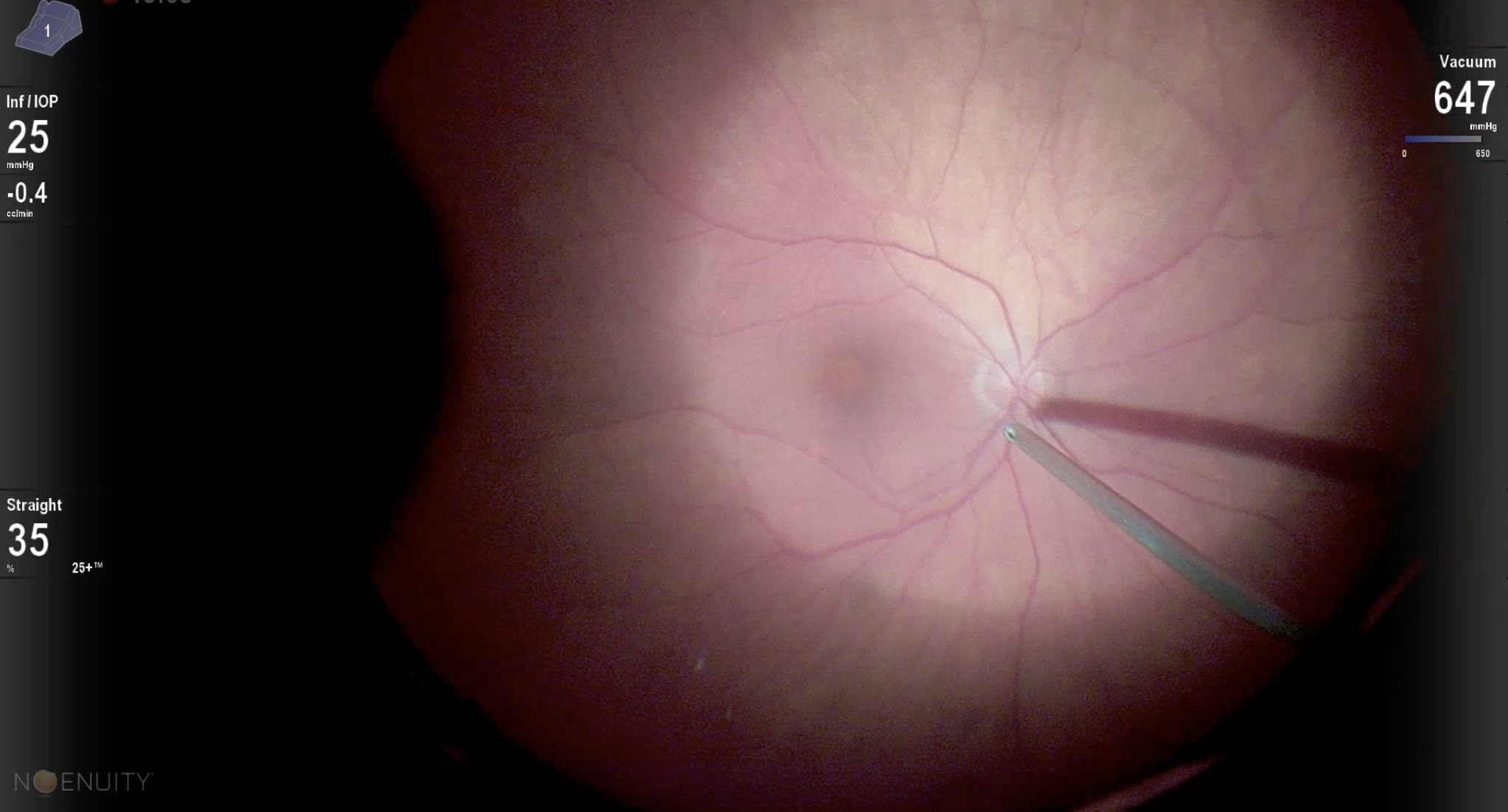
- Place the tip of the vitrectomy cutter to one side of the optic disc (Figure 4.1)
- Aspirate at maximal vacuum (e.g. 650 mmHg) over the optic disc, trying to engage vitreous. This can be facilitated by slowly moving the tip side to side, pausing from time to time
- Once the cutter tip is filled with vitreous, direct the tip tangentially above the retinal surface before gently lifting up. It is safest to elevate the posterior hyaloid nasal to the optic disc first. Carefully observe for elevation of the posterior hyaloid, especially at the leading edge where retinal tears may occur
- If the posterior hyaloid is not elevating, cut to clear the cutter port and repeat the above steps
- The posterior hyaloid only needs to be lifted to the level of the equator. Aggressive lifting risks retinal tears. Once induced, the posterior hyaloid will often continue to gently elevate as the peripheral vitreous is cut
Induction of a PVD may be more difficult under the following circumstances.
- Stronger vitreoretinal adhesion:
- Vitreomacular interface pathology (FTMH and VMTS)
- Diabetes
- Asteroid hyalosis
- Young patients
- When the vitreous has been shaved down close to the retinal surface and optic disc.
In contrast, elderly, pseudophakic patients with epiretinal membranes are more likely to already have a PVD.
- To engage vitreous maximally, it is important to face the cutter port away from the center of the optic disc and direct it radially above the retinal surface before lifting up. This can be repeated in different directions around the optic disc, but each time the cutter port should be turned to face away from the optic disc. Sometimes it’s helpful to engage vitreous along the circumference of the optic disc before pulling away radially
- Stains can be used to visualize the vitreous and assist with PVD induction. This is optional but is useful if PVD induction is difficult or if there is uncertainty if the posterior hyaloid has been elevated. Blue dyes are helpful if the surgeon is already using them for membrane peeling (e.g. epiretinal membranes and macular hole cases). They will sit on top of the optic disc and “wobble” rather than be blown away easily by the infusion cannula when the posterior hyaloid is still attached. The best stain for vitreous however is dilute triamcinolone acetonide (Kenalog®). It can be injected into the vitreous cavity using a soft-tip cannula on a 3ml syringe. Only a small amount needs to be injected directly over the optic disc. Less is more- you want to achieve a “sugarcoating” but no “snowstorm”, otherwise the view will be compromised
- A soft-tip extrusion cannula under a high magnification flat lens can be used to induce a PVD (Figure 4.2). The extrusion vacuum should be set to maximum. The soft-tip has the advantage that it covers a smaller surface area compared to the cutter port, as well as vacuum being applied en face against the retinal surface rather than 90 degrees to it as is the case with the cutter port. Use the soft-tip extrusion cannula to lift the vitreous edge off the optic disc, then the cutter to complete the PVD
- Other instruments including a flex loop, forceps, pick or bent needle can be used to being the PVD induction
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.