5.2.1 PFO Indications and Complications
Perfluorocarbon liquids (PFCL) are a versatile adjunct during vitreoretinal surgery particularly during the management of retinal detachment complicated by proliferative vitreoretinopathy (PVR), giant retinal tears (GRT) or retinal detachment resulting from open globe injury.[1,2,3,4] PFCL are also helpful as a “third hand” in selected types of primary retinal detachment, dislocated lens fragments, and dislocated intraocular lenses as well as IOFBs, and other vitreoretinal manoeuvres. Specifically, perfluoro-n-octane (PFO) is used in the United States but in other countries, perfluorodecalin (PFD) and perfluorophenanthrene are also used. The properties of PFO which make it desirable for intraoperative use are its clarity, a specific gravity of 1.7, a similar viscosity to saline, and a high vapor pressure. It is highly purified for medical application.
To minimize complications from using PFO, it is advised that during vitrectomy, the following instruments also be used:
- Valved cannulas, to decrease the turbulence of the BSS infusion fluid into the eye and minimize the formation of small or peripheral bubbles (“fish eggs”) that can migrate subretinally through a retinal break
- Wide angle or panoramic viewing to be able to visualize the peripheral edge of the PFCL bubble as it nears retinal breaks, as well as to have excellent visualization during fluid-air exchange
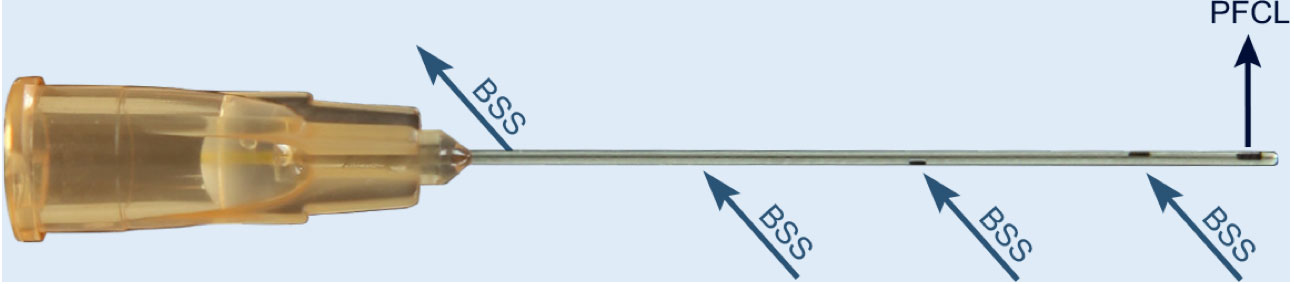
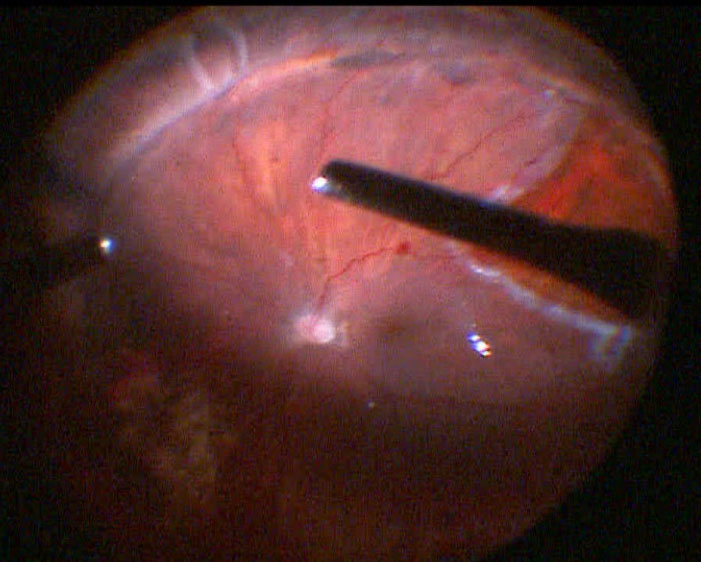
- A dual bore cannula for injection of PFO.[5] The PFO exits from the side of the tip of the cannula. In small gauge vitrectomy, this instrument has several venting sideports along the shaft to reduce the intraocular pressure during injection (Figure 5.2.1)
Chang S, Kwun RC. Perfluorocarbon Liquids in Vitreoretinal Surgery in RETINA (ed. Ryan SJ, Wilkinson CP) Chapter 128, pp 217-2190, 4th Edition, 2006. Elsevier-Mosby (St. Louis)
Coll GE, Chang S, Sun J, Wieland MR, Berrocal MH. Perfluorocarbon liquids in the management of retinal detachment with proliferative viteoretinopathy. Ophthalmology 1995; 102:630-639.
Gonzalez MA, Flynn Jr HW, Smiddy WM, Albini TA, Tenzel P. Surgery for retinal detachment in patients with giant retinal tear: etiologies, management strategies, and outcomes. Ophthal. Surg Laser Imaging Retina 2013; 44:232-237.
Chang S, Reppucci V, Zimmerman NJ, Heinemann MH, Coleman DJ. Perfluorocarbon liquids in the management of Traumatic retinal detachments. Ophthalmology 1989; 96:785-791.
Toygar O, Berrocal MH, Martin C, Riemann CR. Next-generation dual bore cannula for injection of vital dyes and heavy liquids during pars plana vitrectomy. Retina 2016; 36:582-587.
- High pressure tubing allows for an assistant to hold the syringe and control the injection speed while the surgeon manipulates the cannula. This allows for greater control of the large syringe. The VFC cannula on a low injection pressure can also be used to control PFO injection with the foot pedal
- PFO should be injected when the retina is mobile, and preferably when the retinal breaks are seen. In cases of a “closed or narrow funnel” configuration in PVR, a viscoelastic (e.g. Healon®) would be a better tool to open up the retinal folds for posterior epiretinal membrane peeling. Once the posterior preretinal membranes are removed and the retina is mobile, PFO can be used to flatten the retina
- Be sure a posterior vitreous detachment has been confirmed before injecting PFO as the bubble may trap the hyaloid if not previously elevated
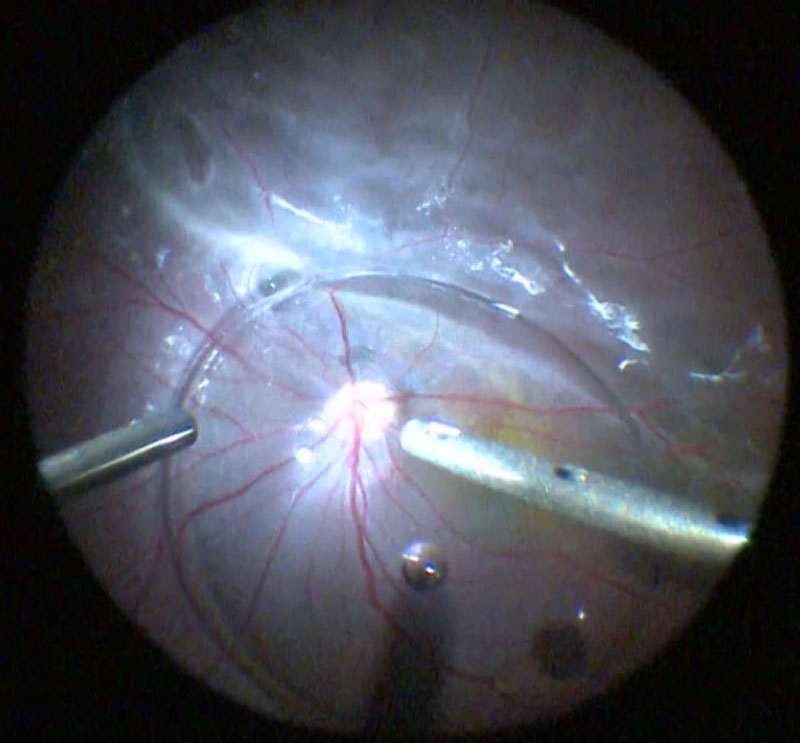
- When injecting PFO, the injection should be slow, maintaining the tip of the injection needle within the PFO bubble so it grows as one large bubble. The optic disc should be observed and if the central retinal artery closes or pulsates, the rate of injection should be slowed. Watch the retina flatten. It is not necessary to fill the vitreous with one injection – inject to a comfortable level, and then add PFO as necessary during the operation (Figure 5.2)
- When inserting or withdrawing the injection cannula, keep the tip away from retinal breaks to minimize the chance that some drops of PFO could leak and pass subretinally through retinal breaks. Consider injection through a trocar where the canula does not need to traverse a large retinal break if possible. Always maintain a degree of negative pressure on the syringe while traversing retina prior to the reaching the injection site as without negative pressure, PFO often leaks out of the canula. When performing fluid-air exchange also always keep a slight negative pressure on the extrusion canula at all times when entering and exiting the eye to prevent unintentional PFO leakage
- When injecting, make sure to roll / “squeegee” the fluid out by rocking and injecting the PFO first on the area where there is less subretinal fluid
- In addition to avoiding a posterior retinotomy, the PFO flattens the posterior retina and reduces mobility of the retina so that vitreous traction can be thoroughly removed from the flap of retinal tears and the peripheral vitreous can be shaved down. It thus aids in vitrectomy in sticky hyaloids where the retina also happens to be highly mobile
- As the PFO level rises be aware that mechanical manipulation of the globe (e.g. scleral depression) may cause PFO bubbles to form at the peripheral surface. Reduce the infusion pressure if bubbles frequently form
- Make sure to remove all traction over retinal breaks before lifting PFO over the break as a break with unrelieved traction will act as a sink for subretinal PFO
As PFO fills the eye:
- Residual preretinal membranes can be visualized and peeled under PFO
- Shave peripheral vitreous down to reduce the potential for anterior PVR (Figure 5.2.3)
- Examine the retinal periphery for any retinal breaks, or signs of residual traction that requires a relaxing retinotomy or membrane peeling. If the PFO is unable to flatten the retina in an area, this suggests some residual traction exists. In these cases, PFO often adopts an ovoid rather than a spherical configuration
- If a small peripheral break cannot be located, PFO can displace the subretinal fluid through the break and reveal it (“Schlieren phenomenon”). Diluted trypan blue can also be injected subretinally using a 41-gauge cannula and when PFO flattens the retina, the blue fluid exits through the retinal break
- In eyes with retinal incarceration following open globe injury, shave vitreous completely at the incarcerated site
- If all traction on the retina has been released, PFO can be added above the level of any retinal breaks. This facilitates laser of the breaks (especially retinotomies) since visualization is better (Figure 5.2.4)
- Laser under PFO where possible to treat the retinal breaks and the laser burns will make the retinal breaks more visible during fluid-gas exchange. Additional laser photocoagulation is often necessary under air (when the view will widen) to treat the most anterior aspects of the break
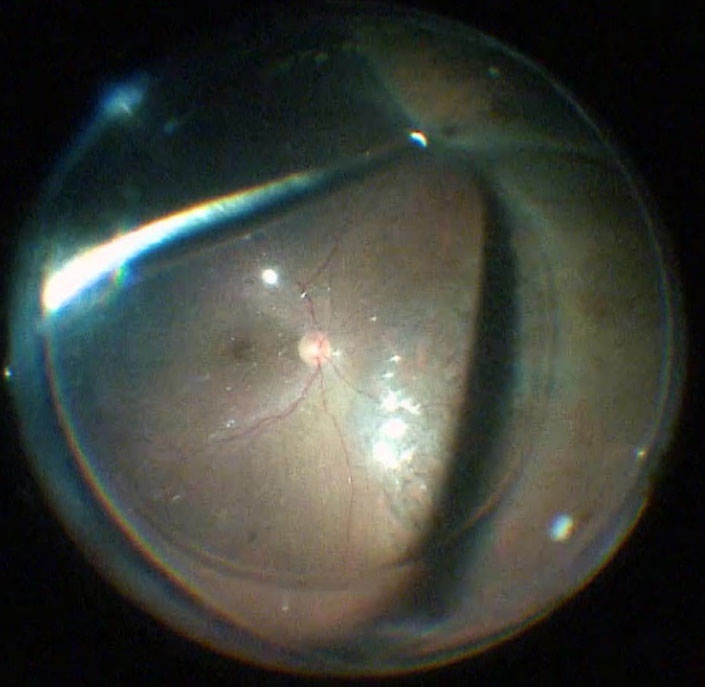
Place the soft-tip cannula near the most posteriorly located retinal break, and begin aspirating peripheral anterior vitreous fluid (active or passive aspiration). As the air comes into the eye, the anterior retina flattens and subretinal fluid will be displaced back into the vitreous. When the anterior retina is flat, begin to aspirate the PFO starting at the top surface of the bubble. You might have to return to internal aspiration of subretinal fluid if some becomes visible. If the break is at the ora serrata, PFO can be filled all the way to the ora serrata and the fluid-air exchange can be performed there. If the break is posterior, PFO can be filled to the most posterior break and the fluid air exchange can be performed there. Any subretinal fluid anterior to the PFO bubble will be pushed out of the break as air enters anterior and the extrusion canula continues to aspirate at the break (Figure 5.2.5).
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.