Chapter 24
Stem Cell Therapy
Stem cells constitute cell populations with unlimited self-renewal and differentiation abilities, which can potentially generate any cell type. These properties have made them a promising treatment for degenerative eye disorders that lead to blindness. Currently, stem cell delivery is not an approved standard of care treatment for retinal diseases. Early human clinical trials have begun, mainly for stem cell derived retinal pigment epithelium (RPE), to assess preliminary efficacy and safety considerations (including the possibility of neoplastic cell growth and unrestricted proliferative changes). It is hoped that these and future neuro-retinal replacement strategies will progress to treatments in the coming years.
Note: Feasibility of Ocular Stem Cell Delivery
- Ease of access to ocular tissues
- Need of low stem cell dose given the small size of the eye
- Limited response to external antigens due to immune privilege state
- Easy detection and monitoring of functional and anatomical changes after administration
- Possibility to remove or destroy the transplanted tissue (to some extent) if adverse events arise
The steps required to achieve a stem cell-based treatment are:
Candidates include those characterized by progressive degeneration of the photoreceptor-RPE cell complex or retinal ganglion cells, for example:
1.Acquired retinal diseases
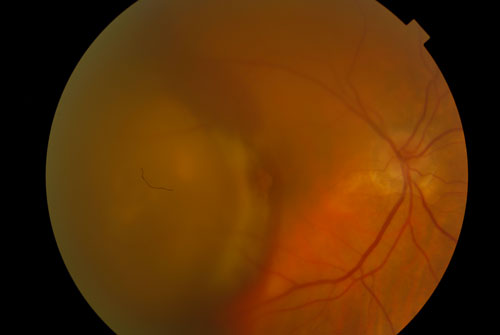
- Age Related Macular Degeneration (Figure 24.1)
- Degenerative myopia
- Optic nerve disease
- Retinitis Pigmentosa
- Stargardt’s disease
- Best disease
- Leber’s congenital amaurosis
- Promoting survival of host cells to preserve function (through the influence of trophic factors)
- Replacement therapy of specific cell types to restore function
The use of autologous cells, in theory, should not pose a risk of a severe immunological response compared to an allogenic source. However, stem cells may trigger T-cell mediated immunogenicity that could subsequently destroy adjacent tissues and the graft itself. For this reason, appropriate local and/or systemic immunosuppression should be administered concomitantly irrespective of the source type.
Currently, sources available in retinal treatments include:
- Embryonic origin
- Human embryonic pluripotent stem cells (hEPSC) - derived from the inner cell mass of a blastocyst (Figure 24.2)
- Adult origin
- Induced pluripotent stem cells – adult somatic cells that undergo genomic reprogramming to allow development of specific cell lines
- Mesenchymal stem cells: adipose or bone marrow derived
All of these should be ultimately induced to differentiate in the selected target cell to be delivered to the eye (neural retinal cells, photoreceptors or RPE cells).
- Intravitreal injection of stem cells suspension.
- Subretinal
- Stem cells suspension
- Cellular sheet
Ocular
- These depend on complications related to the chosen method of delivery and the inflammatory reaction triggered by the graft, including: progression of cataract, RPE loss, ocular hypertension, lens dislocation, vitreous hemorrhage or vitritis, epiretinal membrane and proliferative vitreoretinopathy formation, choroiditis, retinal detachment, endophthalmitis and tumor growth, among others.
Systemic
- Related to potential extraocular tumor formation and immunosuppressive drugs
Function
- Best corrected visual acuity
- Low luminance visual acuity
- Contrast sensitivity
- Microperimetry
Structure
- Full ophthalmic examination
- Retinal imaging (Figure 24.3)
- Fundus autofluorescence
- Optical coherence tomography
- Fundus fluorescein angiography
- Adaptive optics scanner laser ophthalmoscopy
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.