Chapter 22
Vitrectomy with Keratoprosthesis
The keratoprosthesis (KPro) provides a clear visual axis in forms of corneal opacification that are not amenable to penetrating keratoplasty.[1-6] The KPro can achieve rapid visual rehabilitation, but the potential for complications including retroprosthetic membrane, glaucoma, retinal detachment, and endophthalmitis necessitates a team-based approach. A primary pars plana vitrectomy (PPV) with glaucoma valve implant at the time of KPro implantation can prevent the development of anterior vitreous traction, allow for immediate visualization and treatment of the retina, and prevent glaucoma progression. Pars plana tube placement is recommended as the anterior chamber may become scarred and difficult to visualize after KPro.[1] The Boston Type I KPro, which has a collar button design with a front plate with optical stem, donor corneal ring, and back plate, is the most commonly used keratoprosthesis in the United States (Figure 22.1).
Vajaranant TS, Blair MP, McMahon T, Wilensky JT, de la Cruz J. Special considerations for pars plana tube-shunt placement in Boston type 1 keratoprosthesis. Arch Ophthalmol. 2010 Nov;128(11):1480-2. PubMed PMID: 21060051. Epub 2010/11/10. eng.
Ray S, Khan BF, Dohlman CH, D'Amico DJ. Management of vitreoretinal complications in eyes with permanent keratoprosthesis. Arch Ophthalmol. 2002 May;120(5):559-66. PubMed PMID: 12003604. Epub 2002/05/11. eng.
Kiang L, Sippel KC, Starr CE, Ciralsky J, Rosenblatt MI, Radcliffe NM, et al. Vitreoretinal surgery in the setting of permanent keratoprosthesis. Arch Ophthalmol. 2012 Apr;130(4):487-92. PubMed PMID: 22491917. Epub 2012/04/12. eng.
Harissi-Dagher M, Durr GM, Biernacki K, Sebag M, Rheaume MA. Pars plana vitrectomy through the Boston Keratoprosthesis type 1. Eye (Lond). 2013 Jun;27(6):767-9. PubMed PMID: 23579405. Pubmed Central PMCID: PMC3682363. Epub 2013/04/13. eng.
Behlau I, Martin KV, Martin JN, Naumova EN, Cadorette JJ, Sforza JT, et al. Infectious endophthalmitis in Boston keratoprosthesis: incidence and prevention. Acta Ophthalmol. 2014 Nov;92(7):e546-55. PubMed PMID: 24460594. Epub 2014/01/28. eng.
Aldave AJ, Kamal KM, Vo RC, Yu F. The Boston type I keratoprosthesis: improving outcomes and expanding indications. Ophthalmology. 2009 Apr;116(4):640-51. PubMed PMID: 19243830. Epub 2009/02/27. eng.
Vajaranant TS, Blair MP, McMahon T, Wilensky JT, de la Cruz J. Special considerations for pars plana tube-shunt placement in Boston type 1 keratoprosthesis. Arch Ophthalmol. 2010 Nov;128(11):1480-2. PubMed PMID: 21060051. Epub 2010/11/10. eng.
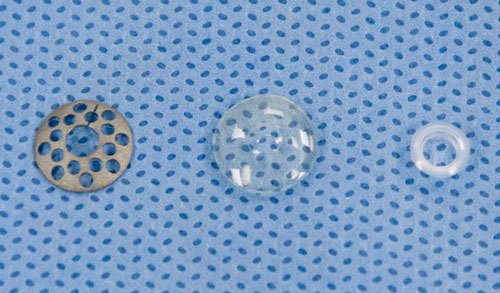
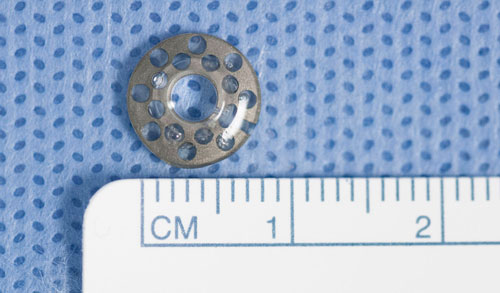
Figure 22.1
A.The Boston Type I Keratoprosthesis consists of a back plate, corneal tissue, and front plate with optical stem, depicted from left to right.
B. Front view and
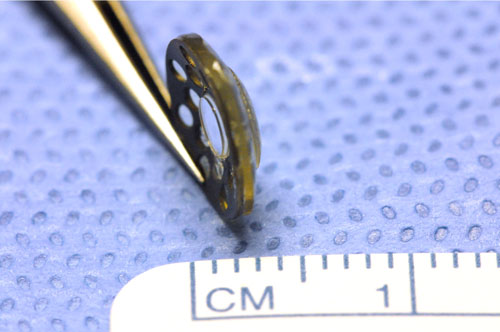
C. Side view
of an assembled Boston Type 1 Keratoprosthesis.
C
Figure 22.1
A.The Boston Type I Keratoprosthesis consists of a back plate, corneal tissue, and front plate with optical stem, depicted from left to right.
B. Front view and
C. Side view of an assembled Boston Type 1 Keratoprosthesis.
1. Preoperative Evaluation
- Patient selection. An understanding of the visual prognosis, need for a multidisciplinary approach, and commitment to lifelong care of the KPro, eye safety, medications, and long term follow up are critical to the success of the KPro
- Pre-operative physical. General anesthesia is preferable
- Assessment of conjunctival mobility for a glaucoma implant
- Axial length to determine the necessary KPro refractive power
- B-scan. Evaluation of posterior segment as corneal opacification often precludes indirect ophthalmoscopy[2]
- Endoscopy is a good tool at the start of the case to determine if there is visual potential prior to proceeding with the entire surgery
Ray S, Khan BF, Dohlman CH, D'Amico DJ. Management of vitreoretinal complications in eyes with permanent keratoprosthesis. Arch Ophthalmol. 2002 May;120(5):559-66. PubMed PMID: 12003604. Epub 2002/05/11. eng.
2. Glaucoma Shunt Placement
- 360-degree conjunctival peritomy and opening of 4 quadrants
- The glaucoma valve is secured to the sclera superotemporally
- The tube is tucked underneath the plate
3. Infusion Cannula and Sclerotomies
- Placement of the infusion cannula and valved trocars prior to the KPro allows for better visualization of landmarks and obviates the need for Flieringa ring. Aim for 3 mm posterior to limbus. Occasionally, determination of the limbus may be difficult. In these scenarios, assume a previous corneal diameter of 10 - 11mm. This represents a distance of 5 - 5.5mm from the center of the optic to the limbus. Sclerotomies placed too anterior will result in instrumentation being blocked by the KPro, and may damage the back plate, hampering visualization
- A longer (6 mm) infusion cannula aids visualization through the KPro optic
- The superotemporal sclerotomy should be placed more inferiorly to allow for placement of the glaucoma tube
- The infusion can be turned on as soon as visualized, usually after removal of the host cornea
4. Keratoprosthesis Placement
- The KPro is implanted. Intraocular lens explantation if present
- An alternative to starting with the KPro placement is to first place a temporary keratoprosthesis, then proceed with the vitrectomy and finally replace the temporary keratoprosthesis with the permanent keratoprosthesis. This approach allows for wider field visualization during the vitrectomy
- If placing a glaucoma drainage implant, the glaucoma surgeon may prefer to begin the case with conjunctival peritomy
5. Pars Plana Vitrectomy
- Smaller incisions are preferable in the setting of conjunctival scarring.[3] The stiffer 23-gauge instrumentation aids in manipulation
- Contact and non-contact lens systems can provide adequate visualization for pars plana vitrectomy with a KPro.[3,4] Contact lens viewing allows improved visualization of the periphery
- A thorough PPV and vitreous base shave should be performed, especially around the site of the pars plana tube insertion. Scleral depression is often not helpful in the setting of a KPro
- Scleral depression may be useful if performing the vitrectomy under a temporary keratoprosthesis; however, care should be taken to avoid aggressive shaving as an iatrogenic break may significantly influence the completion of the other portions of the case
- If no posterior vitreous detachment is present, one can be induced if facile
- Of note, air-fluid exchange can be performed with a Boston KPro without excessive fogging[4]
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.