Chapter 28
Choroidal Drainage
Choroidal detachments can be serous, hemorrhagic, or a mixture of both. They often occur in the setting of post-operative hypotony, such as following trauma or glaucoma surgery. In most cases serous choroidal effusions will settle spontaneously and do not require surgery. Indications for drainage of choroidals include:
- Development of hypotonous maculopathy
- “Kissing” (touching) choroidal detachments causing retinal apposition
- Massive suprachoroidal hemorrhage (SCH)
- Uncontrolled intraocular pressure (associated with SCH)
- Severe shallowing of the anterior chamber causing corneo-lenticular touch
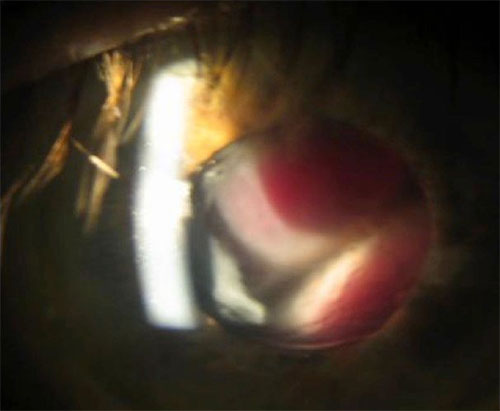
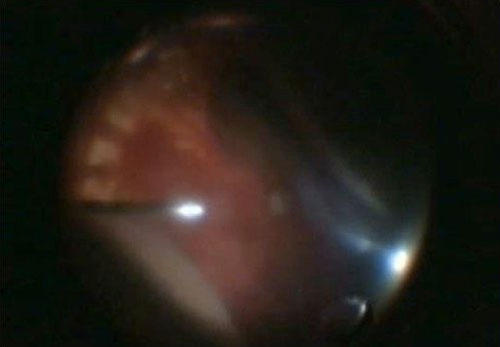
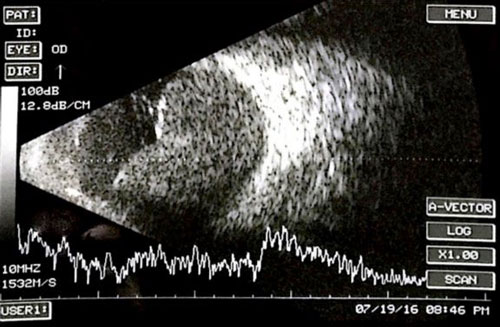
Examples of suprachoroidal hemorrhage are shown in Figures 28.1-28.3 below:
In the case of SCH, it is advised to wait 7-14 days to allow the blood to liquefy- this can be confirmed on B-scan ultrasonography. If SCH occurs intra-operatively during a vitrectomy, increase the intraocular pressure (IOP) to tamponade the hemorrhage and suture the sclerotomies. Silicone oil tamponade may be required.
1. Anterior Chamber Maintainer
In most cases it is best to insert an anterior chamber infusion line (Figure 28.4A). Initiating placement of the infusion line through the pars plana risks suprachoroidal infusion, worsening the situation. Intraocular pressure is increased in a controlled fashion to allow for extrusion of suprachoroidal blood through the sclerostomy.
2. Scleral Cut-downs
Perform a conjunctival peritomy and diathermy to the sclera. Using a hockey stick “Beaver®” type (scleral) blade, a 1-2mm sclerotomy is made 3 to 4 mm from the limbus in a radial fashion in the quadrant where there is a largest collection of blood (Figure 28.4B). i.e. highest point of SCH. Care is taken to place it anterior to the vortex veins. A 27-gauge needle can be used to externally drain the hemorrhage. Clots can be evacuated using a cyclodialysis spatula. Cotton buds / q-tips can be used to “milk” the blood (Figure 28.4C & Figure 28.4D). Aggressive drainage may risk retina incarceration.
An alternative method is to use the trocar MVR style blade 4mm posterior to the limbus in a stab style incision. If the first drainage is unsuccessful, consider trying another location slightly more posterior (up to 7mm posterior to the limbus). Preoperative ultrasound to determine the highest extent of the hemorrhage may be useful in determining where to drain.
3. Sclerotomies
A long (6mm) pars plana infusion cannula is preferred and must be seen through the pupil before being switched on. Care must be taken to avoid traumatising prior glaucoma surgery (e.g trabeculectomy or glaucoma drainage device, if this preceded the choroidal detachments). If a glaucoma surgery was related to the hemorrhage via hypotony, the glaucoma specialist should be consulted to determine whether closure of any drainage devices is warranted.
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.