26 Lens Management
26.1 Phaco-Vitrectomy
26.2 Pars Plana Lensectomy
26.3 Intraocular Lens Explantation
26.4 Secondary Intraocular Lens Insertion Clinical Scenarios & Clinical Decision Making
26.5 Sulcus Intraocular Lens
26.6 Anterior Chamber Intraocular Lens
26.7 Iris Fixated Intraocular Lenses
26.8.1 Scleral Sutured Intraocular Lens – Traditional 2 Point Fixation
26.8.2 Scleral Sutured Posterior Chamber Intraocular Lens 4 Point Fixation
26.8.3 Scleral Sutured Posterior Chamber Intraocular Lens – “Hoffman” Corneoscleral Pockets
26.8.4 Alternate Technique to Rescue a Dislocated IOL – Triangular Scleral Flap, Sutured IOL Technique
26.8.5 Suturing Without Exchanging the Intraocular Lens
26.9 Sutureless Scleral Fixation of an Intraocular Lens
26.8.4 Alternate Technique to Rescue a Dislocated IOL – Triangular Scleral Flap, Sutured IOL Technique
Advantages of IOL repositioning include generally less morbidity (no need for anterior incisions and corneal endothelial cell loss-inducing traffic through the anterior chamber), and there are many techniques; these commonly share similarities with secondary or exchanges for PC-IOL implantation.
The purpose of this chapter is to describe this author’s technique for scleral suture “rescue” of a dislocated IOL (see accompanying Video 26.8.4 of a one-piece acrylic IOL repositioning with sutures). Additional advantages of this technique include its versatility – it can be performed in the setting of previous glaucoma procedures, previous corneal surgery (penetrating or lamellar keratoplasty), is amenable to use with all caliber vitrectomy systems, and is modifiable for a broad spectrum of PC-IOL styles including multifocal lenses.
The surgical steps include the following:
- Pre-operatively, it is advisable to measure for an IOL in case it becomes necessary to exchange rather than reposition the IOL
- Conjunctival incisions are made in preparation for fixation, usually at the 1:30 and 7:30 meridians. (This author is right -handed, but a left-handed surgeon would probably want to mirror this by aiming for 4:30 and 10:30 meridians; the ensuing narrative will pertain to a right-handed technique.) If there are pre-existing barriers (previous laceration scars, severe conjunctival scarring, glaucoma hardware) then this position can be modified, but this is the most ergonometrically convenient position for effecting fixation
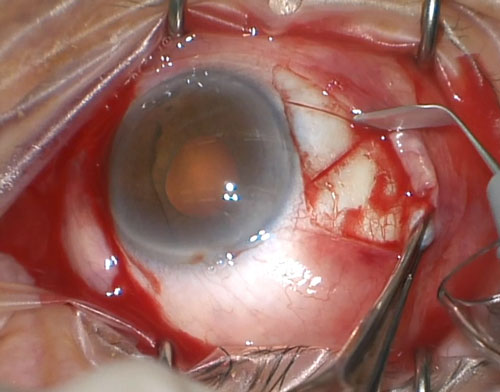
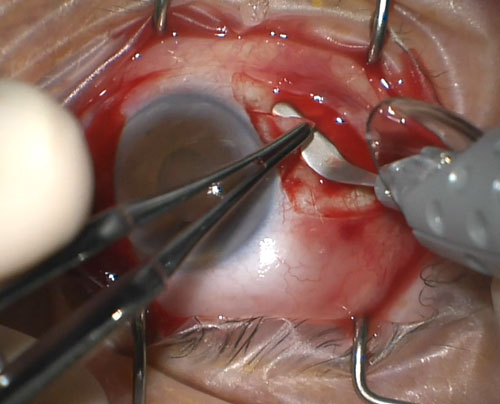
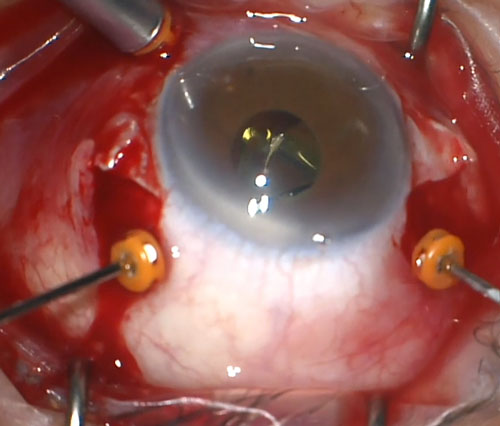
- After cauterizing the superficial sclera, triangular-shaped, limbal-based, about half-thickness scleral flaps are prepared (Figure 26.8.4.1 and Figure 26.8.4.2). It is convenient to make these somewhat larger than one would intend, as the flap seems to contract a bit, and the more posterior the extent, the more posterior the suture knots can be positioned which would seem to lessen the chance for erosion
- For right eyes, it is convenient to place the infusion cannula inferonasally so it is not an impediment to placing the more inferior suture (again, a left-handed surgeon might want to do this for a left eye)
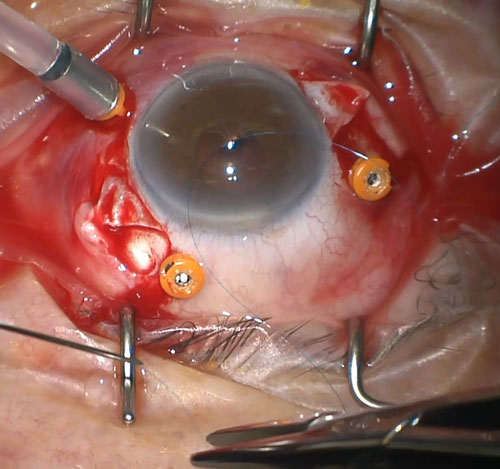
- The 9-0 prolene (using 10-0 prolene has been reported to result in later redislocation with several years of degradation, but this is rare with the slightly larger suture) is threaded retrograde through 27-gauge needles (1/2 inch in length), such that the cut end can be retrieved through the hub of the needle (Figure 26.8.4.3). One of these is prepared for each haptic. Do not pull the suture needle too tightly against the sharp end of the 27-gauge needle- it can break off or be difficult to pull away from the tip when preparing to insert it later
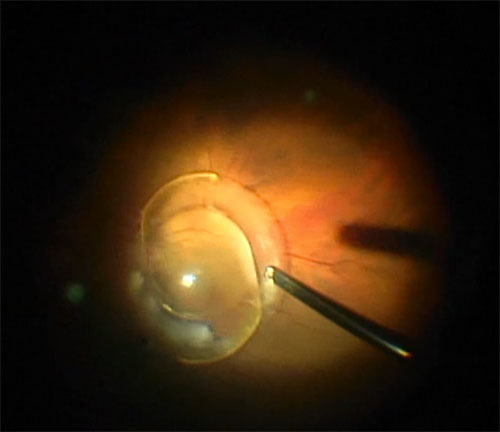
- A core vitrectomy is performed. Judgment regarding how complete to be at this point is necessary. A “balancing act” is that if the IOL is still fairly anterior, it is favorable to gain purchase on it with the forceps (see later step), but one must be cognizant not to try too much manipulation if there is abundant or prolapsed vitreous. If the IOL is grasped in the early stages, then the cutter can be used to remove substantial amounts of mobile and prolapsed vitreous. Beware if a haptic is binding in the vitreous base – it might be necessary to rotate or specifically excise vitreous to mobilize it to avoid vitreous base traction/making a retinal break (Figure 26.8.4.4). If the IOL is completely luxated and is laying on the macula, then a maximal vitrectomy is pursued initially. If there is not a preexisting posterior vitreous detachment (PVD) it can be more difficult to retrieve the IOL so, again, judgment is necessary to free up the IOL and remove as much vitreous as is prudent. It might be best to induce completion of the PVD later, but sometimes this occurs during vitreous removal. It is rare that the IOL can damage the retina in this hydraulic milieu – but not unprecedented
- A key goal is to grasp the IOL with the forceps. Either this has been achieved at the step noted above, or it might be necessary to retrieve the IOL from the posterior pole
- To retrieve an IOL that is posterior, suction from the cutter (held in the right hand) at the edge of the optic (or in some instances the haptic) will usually allow one to lift the IOL anteriorly without retinal trauma. While continuing aspiration, switch the light pipe for the forceps and grasp the IOL more anteriorly with the left hand. The terminal velocity of the IOL, if dropped during this step, is slow enough not to harm the retina on impact, so do not panic if this procedure needs to be repeated to secure the IOL
- This author finds, anecdotally, that the serrated forceps open slightly larger and yield a more stable purchase on the IOL. The IOL is best grasped with the left hand, on the peripheral optic about halfway between the haptics. It might be necessary to hold the IOL in this manner for a moderately lengthy period of time (between effecting more vitreous removal and looping the haptics with the suture), so it is necessary to hold the forceps firmly so as not to lose the grasp on the IOL, but not so firmly as to cut the optic. The imprints seem usually to resolve, or at least not ever be visually impactful
- If this is an endocapsular dislocation, then the IOL is likely encased in substantial cortical and capsular remnant. The first challenge can be to use the cutter to gain enough access to grasp the optic. Once that has been done though, the vast majority of the rest of the remnant should be excised (Figure 26.8.4.5). This can be done with the cutter in the right, alternating between cutting and suction to husk the material off the haptics, while holding the IOL with the forceps in the left hand
- It is important to make sure at this point that the IOL orientation is correct. If it is upside down (haptics emanating to the right) the forceps can just be rotated 180 degrees
- Once the IOL is cleared of remnant lens material and is under control, held with the forceps, the first pre-threaded, suture needle is introduced through the base of the more inferior flap with the right hand. Make sure there is sufficient slack, that the suture needle is at least a half inch away from the tip. Previously, to aim for sulcus fixation, this needle was introduced no more than 1mm from the limbus, but IOL torsion might be less by aiming to be behind the pars plicata by inserting it 3mm posterior to the limbus. Other techniques seem to report good results with this more posterior fixation point also (Figure 26.8.4.6)
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.