15.2 Vitrectomy for Proliferative Diabetic Retinopathy
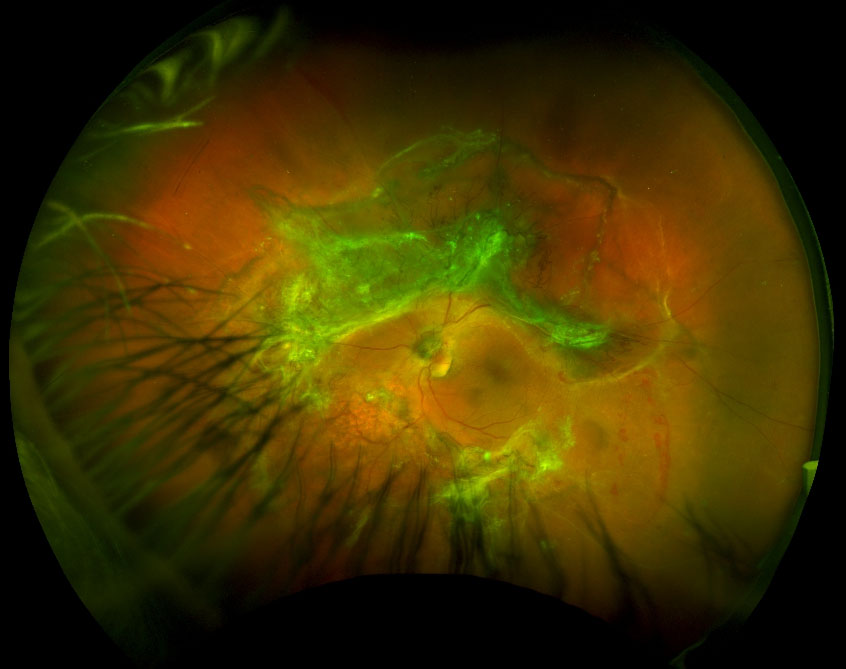
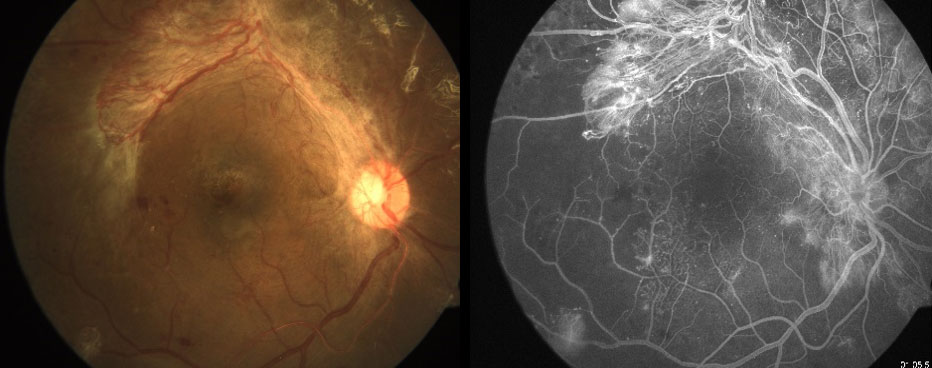
Vitrectomy in eyes with proliferative diabetic retinopathy is one of the most difficult vitreo-retinal operations as they may include a combination of severe pathologies despite relatively good visual acuity (Figure 15.2.1 & Figure 15.2.2). Preoperatively, optical coherence tomography (OCT) biomarkers such as external limiting membrane and ellipsoid zone integrity may help in predicting postoperative visual acuity but other factors like ischemic maculopathy (with adjunctive fluorescein or optical coherence tomography angiography), ischemic optic neuropathy and glaucoma may limit the visual potential.[1]
The timing of surgery depends on the severity and progression of disease, involvement of the fovea by tractional retinal detachment (TRD), status of the fellow eye and systemic health of the patient.
Shah VA, Brown JS, Mahmoud TH. Correlation of outer retinal microstucture and foveal thickness with visual acuity after pars plana vitrectomy for complications of proliferative diabetic retinopathy. Retina. 2012;32(9):1775-80.
Note: Pre-operative Anti-vascular Endothelial Growth Factor (VEGF) Therapy
Consider injecting intra-vitreal anti-VEGF 1-10 days pre-operatively to minimize neovascularization and intra-operative hemorrhage . Some even advocate for several months of anti-VEGF therapy prior to taking the patient for surgery. The advantages include better intraoperative hemostasis, improved surgical planes and more easily disectable membranes. The disadvantages of this include the risk of progression of pre-operative TRD (otherwise known as “crunch”), associated with regression of neovascularization elsewhere (NVE), greater difficulty in identifying NVE intra-operatively (which can re-bleed post-operatively) and the procedural risks of intravitreal injection. Induction of TRD is less likely with neovascularization at the disc (NVD) than elsewhere (NVE)
The presence of significant anterior chamber hyphema in a diabetic patient usually suggests the presence of neovascularization of the iris or angle. This hyphema is often most easily cleared with the vitrector cutter through a paracentesis. Viscoelastic can be injected intracamerally to prevent recurrent hemorrhage blocking the visual axis, impeding visualization of the fundus during vitrectomy. Care must be taken to remove this if the eye is left with a silicone oil fill as the viscoelastic will react with the oil, hastening emulsification. A miotic pupil may need to be dilated pharmacologically, with viscoelastic, by iris stretching (e.g. with Kuglen hooks) or utilising iris hooks. Intracameral anti-VEGF injection may cause regression of rubeosis, reduce the chances of anterior chamber bleeding. A last ditch effort to control anterior segment bleeding during the case is to apply diathermy to the iris vessels but this is often done at the expense of postoperative fibrin deposition.
Vitrectomy at the sclerotomy sites is an essential step, as it prevents the breaks at the sclerotomy site. Remove vitreous (and any hemorrhage) from the core vitreous. This allows for a safe vitrectomy in the event of an underlying retinal detachment. The view of the retina will slowly improve as hemorrhage is removed. In cases with dense subhyaloid hemorrhage, a small opening can be made in the posterior hyaloid, usually nasal to the disc or in an area of maximal bullosity away from the macula and hemorrhage can be aspirated, this helps in obtaining a good view of the underlying retina. Through this hole, the cutter can be introduced and then a 360 antero-posterior release can be performed by working in this plane.
Inspect for:
- Retinal detachment (tractional, rhegmatogenous or combined)
- Foci of NVD/NVE and bridging fibrosis between these
- Prior PRP laser scars
NOTE
Subretinal blood is suggestive of a tear since it does not normally occur in diabetic retinopathy except in exceptional cases when the retina is extremely ischemic
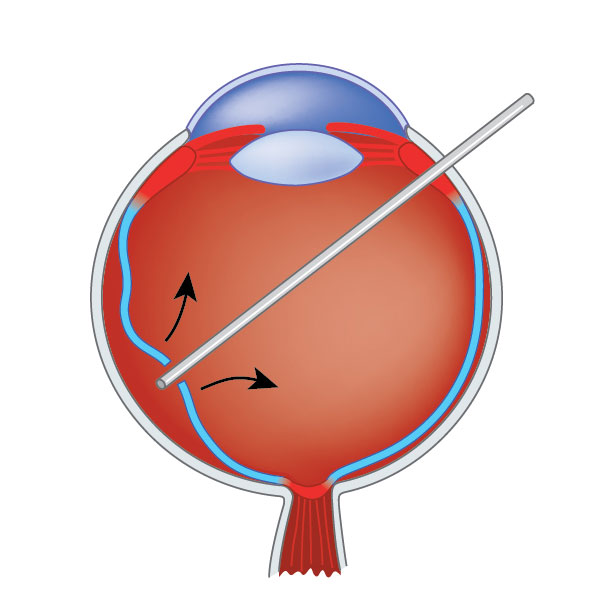
4. Separate the Anterior and Posterior Vitreous (Figure 15.2.3)
Elevation of the posterior hyaloid is an important goal in patients in diabetic vitrectomies. This is thought to reduce the risk of hemorrhage from proliferative disease (as it removes the scaffold for neovascular vessels) and improve oxygenation of the retina, which may improve diabetic macular edema. Patients with proliferative diabetic retinopathy (PDR) often have a very adherent posterior hyaloid, especially in the mid-periphery. Immediate aggressive attempts at elevating the posterior hyaloid may prove unsuccessful and risks tearing the retina. This can particularly occur at sites of NVE where the vitreous is more adherent. It is safest to first separate the anterior and posterior vitreous by cutting vitreous close to the retina in the mid-equatorial region (Figure 15.2.4). Watch for lifting of the anterior vitreous skirt as a sign that this separation has occurred. Dilute intravitreal triamcinolone acetonide is useful for visualization as there is often vitreoschisis and the hyaloid may be stuck down to the periphery.
Elevation of the posterior hyaloid is an important goal in patients in diabetic vitrectomies. This is thought to reduce the risk of hemorrhage from proliferative disease (as it removes the scaffold for neovascular vessels) and improve oxygenation of the retina, which may improve diabetic macular edema. Patients with proliferative diabetic retinopathy (PDR) often have a very adherent posterior hyaloid, especially in the mid-periphery. Immediate aggressive attempts at elevating the posterior hyaloid may prove unsuccessful and risks tearing the retina. This can particularly occur at sites of NVE where the vitreous is more adherent. It is safest to first separate the anterior and posterior vitreous by cutting vitreous close to the retina in the mid-equatorial region (Figure 15.2.4). Watch for lifting of the anterior vitreous skirt as a sign that this separation has occurred. Dilute intravitreal triamcinolone acetonide is useful for visualization as there is often vitreoschisis and the hyaloid may be stuck down to the periphery.
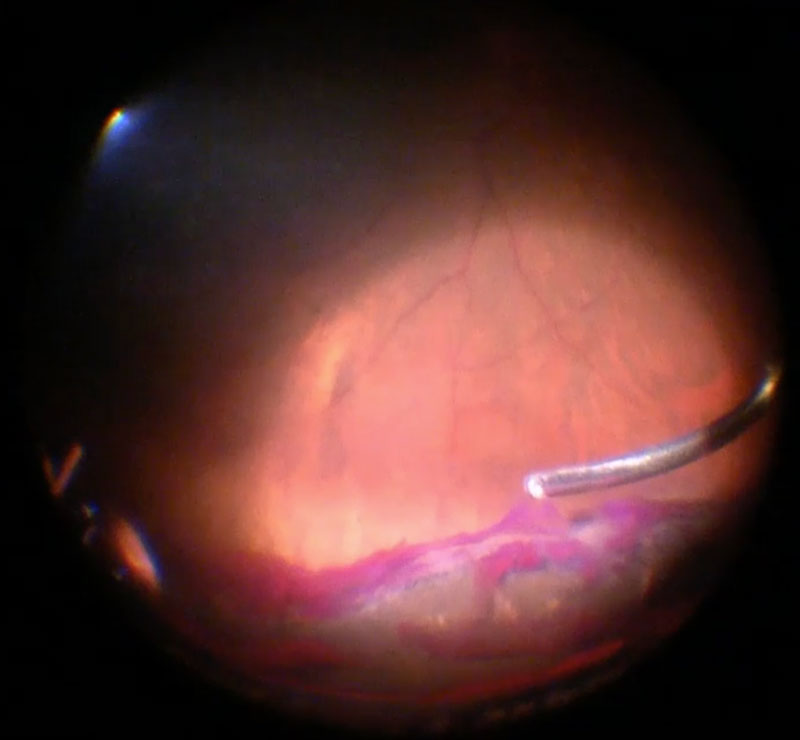
Figure 15.2.3 Vitrectomy for Diabetic Retinopathy
The posterior hyaloid is most adherent at the optic disc, along retinal vessels and at the vitreous base. Vitreo-retinal interface adhesion is often greater in diabetic than non-diabetic patients. By performing vitrectomy in the equatorial region, the anterior and posterior vitreous can be isolated. This makes it safer to elevate the posterior hyaloid without inducing iatrogenic retinal tears.
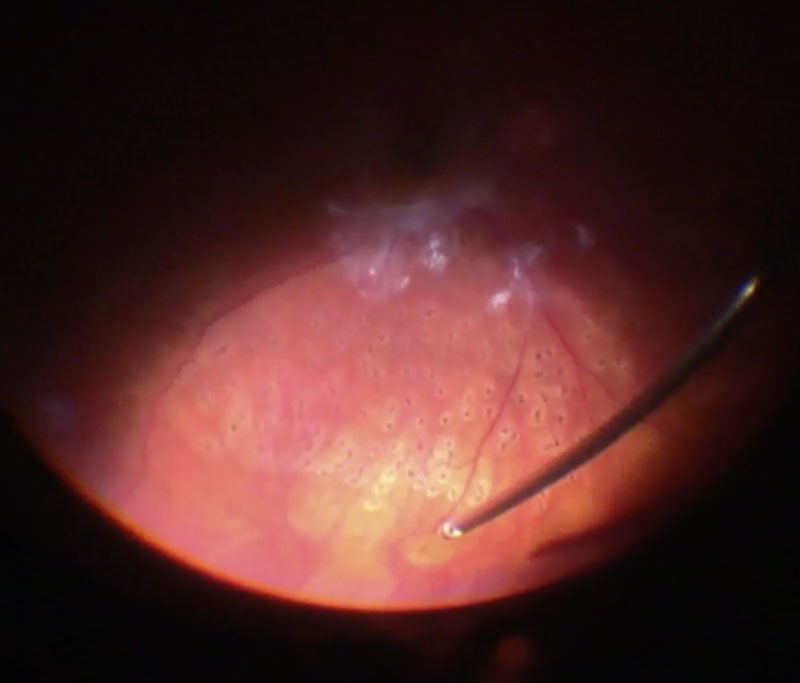
Once the anterior vitreous has lifted, remove this with the cutter. Remove clotted hemorrhage from the vitreous base, as this can lead to post-operative recurrent vitreous hemorrhage. Scleral indentation of the periphery by the assistant may be required to allow for a more complete vitrectomy, particularly in phakic patients (Figure 15.2.5). Cryotherapy should be done in areas of anterior hyaloid proliferation in phakic patients, in pseudophakic and aphakic patients peripheral endolaser can be done.
NOTE
In cases of recurrent vitreous hemorrhage in a previously well lasered eye with PDR, if you see blood stained anterior hyaloid behind the lens always perform a through scleral indentation and look for anterior hyaloid proliferation.
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.