Chapter 1
1 Preoperative Considerations and Anesthesia
Correct patient, correct eye and correct procedure!
- Check informed consent and notes
- Mark eye and dilate pupil
- Perform a “time out” with the anesthetic, nursing and surgical teams
Vitreoretinal surgery can usually be performed under local anesthesia (LA). Choices include retrobulbar, peribulbar, sub-Tenon’s and topical anesthesia. Selecting which type depends on personal preference, prior training and at which stage of the surgery it is required. Commonly, the most painful steps of surgery are the insertion of trocars, scleral depression, cryotherapy and scleral buckling. Better akinesia may be an advantage of peri- and retrobulbar blocks (Figure 1.2), but the latter has been associated with a higher risk of globe perforation and brainstem anesthesia. This has led to a reduction in popularity of retrobulbar LA and increased enthusiasm for sub-Tenon’s LA (Figure 1.3), especially in long eyes. Incomplete or insufficient LAs can be supplemented during the surgery. Mild sedation is helpful during insertion of the LA as well as during the procedure.
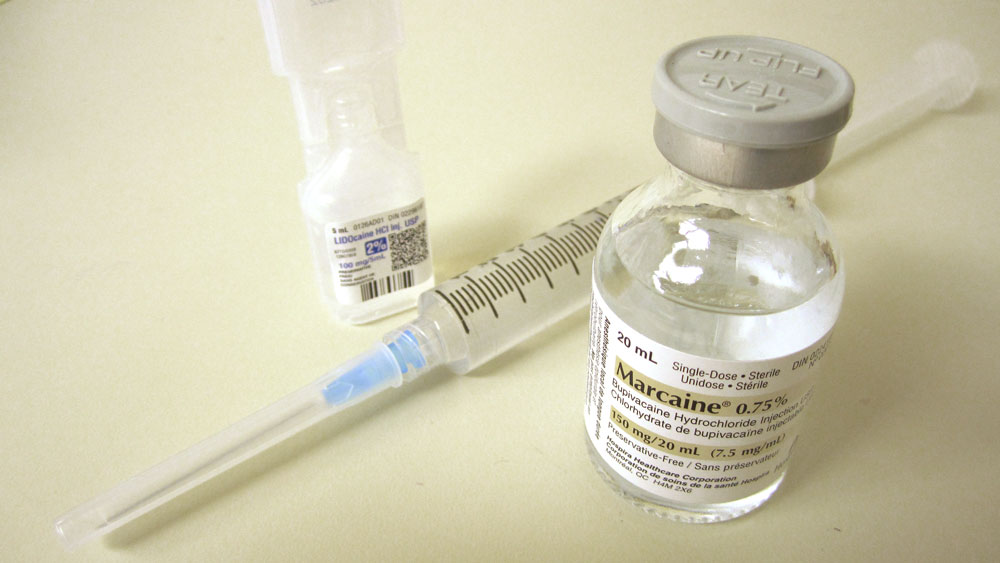
Commonly used medications for performing LA include combination of 2% lignocaine and 0.75% bupivacaine hydrochloride, or pure 1% ropivacaine hydrochloride.
(Figure 1.1). Both these options offer good efficacy of anesthesia, with no significant differences in volume of anesthetic required, time to onset of block, perioperative pain scores or frequency of adverse events.[1] However, the lower potential for systemic toxicity of ropivacaine compared with bupivacaine may be advantageous.[2]
Indications for general anesthesia (GA) include children, the non-compliant patient (e.g. dementia or mental retardation), involuntary movements (e.g. head tremor), extreme claustrophobia or anxiety, and globe rupture. It may also be safer in extremely high axial myopes to avoid the risk of globe perforation associated with LA. GA is also preferable for longer procedures (e.g. combined vitrectomy / scleral buckling surgery).
Pre-anesthesia baseline readings of blood pressure, oxygen saturation and ECG should be obtained.
McLure HA, Rubin AP, Westcott M, Henderson H. A comparison of 1% ropivacaine with a mixture of 0.75% bupivacaine and 2% lignocaine for peribulbar anaesthesia. Anaesthesia. 1999 Dec;54(12):1178-82. doi: 10.1046/j.1365-2044.1999.01069.x. PMID: 10594416.
Markham A, Faulds D. Ropivacaine. A review of its pharmacology and therapeutic use in regional anaesthesia. Drugs. 1996 Sep;52(3):429-49. doi: 10.2165/00003495-199652030-00012. PMID: 8875132.
Performing a Peri-/Retrobulbar Block
A common LA preparation is a 50:50 combination of 2% lignocaine and 0.75% bupivacaine hydrochloride (Marcaine®), or pure 1% ropivacaine hydrochloride (Naropin®). Hyaluronidase (Hylase® e.g. 500 IU) can be added but can be associated with allergic reactions. The solution should be drawn up in a 10ml syringe on a 25-gauge 25mm (peribulbar) needle. The approach may be transconjunctival or through the skin.
- Clean the lower eyelid with povidone iodine (Betadine®) or an alcohol wipe (or irrigate the conjunctival sac with povidone iodine after instilling topical anesthesia).
- Ask patient to maintain primary gaze (in the supine position)
- For transcutaneous injections, using the index finger of your non-injecting hand, feel for the space between the globe and the inferior orbital rim. Keep this finger in place to push the globe superiorly away from the needle tip. Enter the lower eyelid in a natural lid crease at the junction of the lateral 1/3 and medial 2/3. For a transconjunctival approach, pull the lower lid down and enter the inferior fornix at the lateral 1/3
- Aim directly posteriorly for the first 1cm, then angle the needle tip slightly superiorly and medially, letting the needle “sink in” with gravity
- Ask patient to look left, then right, then back to primary. If the needle tip is caught on a rectus muscle it will move. If this occurs, reposition the needle.
- Aspirate to check that the needle tip is not in a blood vessel (when blood will be drawn) or intrathecally (when CSF will be drawn)
- Inject slowly, feeling for increasing tightness of the orbit and watching for ptosis to know when to stop. A typical administration requires between 4 – 10ml (cc). Less is required for most Asian orbits, which are usually smaller. Excess block volume risks central retinal artery occlusion, and easy collapse of the eye during vitrectomy
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.