26 Lens Management
26.1 Phaco-Vitrectomy
26.2 Pars Plana Lensectomy
26.3 Intraocular Lens Explantation
26.4 Secondary Intraocular Lens Insertion Clinical Scenarios & Clinical Decision Making
26.5 Sulcus Intraocular Lens
26.6 Anterior Chamber Intraocular Lens
26.7 Iris Fixated Intraocular Lenses
26.8.1 Scleral Sutured Intraocular Lens – Traditional 2 Point Fixation
26.8.2 Scleral Sutured Posterior Chamber Intraocular Lens 4 Point Fixation
26.8.3 Scleral Sutured Posterior Chamber Intraocular Lens – “Hoffman” Corneoscleral Pockets
26.8.4 Alternate Technique to Rescue a Dislocated IOL – Triangular Scleral Flap, Sutured IOL Technique
26.8.5 Suturing Without Exchanging the Intraocular Lens
26.9 Sutureless Scleral Fixation of an Intraocular Lens
26.9 Sutureless Scleral Fixation of an Intraocular Lens
Recently, a technique for trans-conjunctival, sutureless scleral fixation of an intraocular lens has been described. The method was reported by Shin Yamane 2017.[1] This technique can be used with any 3-piece intraocular lens (IOL), such as:
A. Zeiss ® CT Lucia 202 (Spheric) or 602 (Aspheric, Formerly EC-3 PAL, Only Available in the USA).
This IOL has the advantage that it has polyvinylidene fluoride (PVDF) haptics. These haptics are more forgiving and kink less easily than PMMA haptics. Treat the haptics carefully, as abrupt movements and pulling may cause haptics to kink or disengage from the optic, which will require explantation of the IOL.B. Alcon® MA60 IOL
C. Tecnis® ZA9003
The technique can be used to rescue a dislocated 3-piece IOL, during IOL exchange, or in an aphakic eye.
Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017 Aug 1;124(8):1136-42.
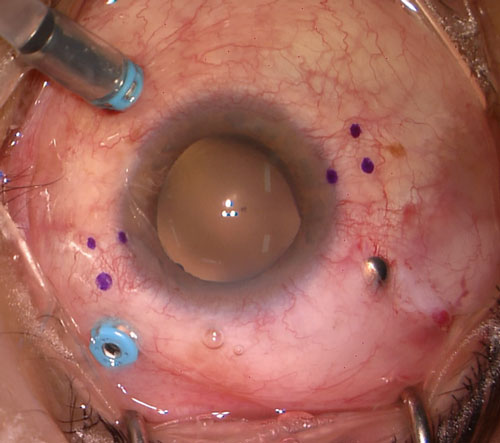
Mark the horizontal meridian of the eye at the corneal limbus using a toric marker. Mark 2mm posterior to this on each side, then 2mm superior to this mark on the left-hand side (temporal for left eye) and 2mm inferior to this mark on the right-hand side (nasal for right eye) (Figure 26.9.1).
Figure 26.9.1 Pen Marks Have Been Made Across the Horizontal Meridian and 2mm Posterior to the Limbus
Further marks are made 2mm superior to this on the left-hand side and 2mm inferior to this on the right-hand side. In this case a 20-gauge superonasal sclerostomy (with silver plug) has been created to allow for fragmentation of a dislocated crystalline lens.
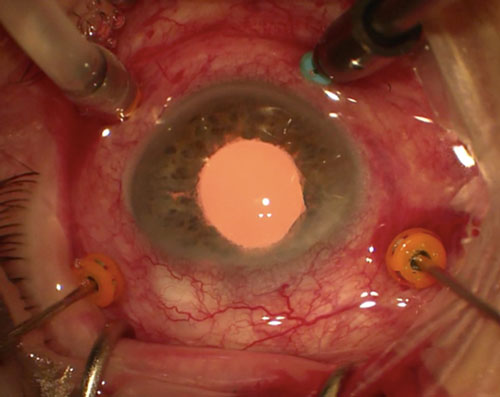
Perform a standard 3-port 25-gauge or 27-gauge (if feeding the IOL haptics through the cannulae) pars plana vitrectomy with optional fourth port for chandelier endoillumination to allow for bimanual manipulation of the IOL. Sutureless scleral fixated IOLs can be performed via cannulae or needles (Figure 26.9.2):
A. Needles
Consider the entry sites for the IOL fixation when placing the vitrectomy trocars to leave enough space for manipulating the IOL.
B. Cannulae[2]
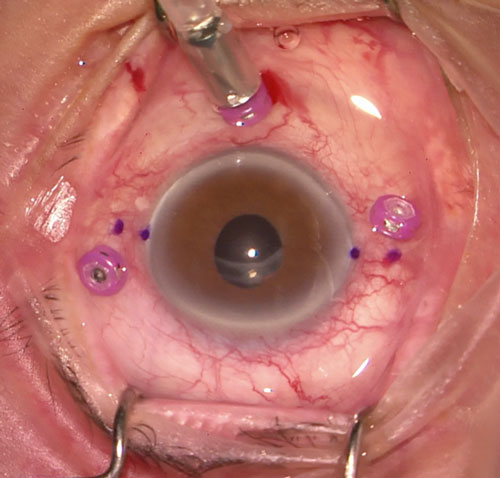
The haptics can be passed through two 27-gauge cannulae instead of needles. It is important that the cannulae are tunnelled as long as possible, and in opposite directions on each side. It is easier to scleral tunnel fixate the IOL than with needles, but the IOL may not be as secure since the cannulae and subsequent scleral tunnels are larger (27-gauge) than 30-gauge needles (Figure 26.9.3).
Abbey AM, Hussain RM, Shah AR, Faia LJ, Wolfe JD, Williams GA. Sutureless scleral fixation of intraocular lenses: outcomes of two approaches. The 2014 Yasuo Tano Memorial Lecture. Graefe's Archive for Clinical and Experimental Ophthalmology. 2015 Jan 1;253(1):1-5.
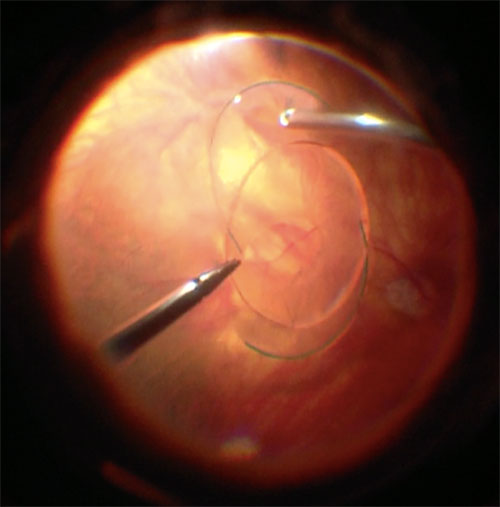
If there is retained lens material or a dislocated IOL that needs to be removed (e.g. single piece), this should be done first. See Chapter 26.2 Pars Plana Lensectomy and Chapter 26.8.1 Scleral Sutured IOL- Traditional 2 Point Fixation. If a 3-piece IOL with is already present, use the cutter to free it from any capsule so that it can be re-utilized for scleral fixation (Figure 26.9.4).
This step can be omitted if a dislocated 3-piece IOL is being rescued or a scleral tunnel is created instead.
A. Needles
Insert thin walled 30-gauge needles (e.g. TSK ultra-thin wall needle; Tochigi Seiko, Tochigi, Japan) in a beveled fashion 2.0 mm posterior to the limbus at the 3 o’clock meridian aiming inferiorly. The needle should be tunneled for 2.0mm before being turned into the eye. It is best to bend the needle prior to insertion so that it lies in the correct plane. It is often easiest to place a 1ml (cc) syringe on the end of the needle to be used as a handle. The long surface of the beveled needle should lie inferior, away from the surgeon.
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.