8 Rhegmatogenous Retinal Detachment Concepts
8.3 Proliferative Vitreoretinopathy
Proliferative vitreoretinopathy (PVR) is a fibrotic disease caused by a complex cellular reaction representing a vitreo-retinal wound healing response that results from a retinal injury. It is the leading cause of failure of retinal detachment surgery. It occurs in approximately 10% of all retinal detachments. [1] Appropriate management of a retinal detachment at the first operation is crucial, as the risk of proliferation and re-detachment increases with each subsequent surgery. Studies on risk factors for PVR are difficult to interpret and have often yielded contradictory results. In general, PVR risk increases with:[1,2,3]
- Prior failed retinal detachment repair
- Pre-operative PVR
- Larger breaks (over 3 optic discs or giant retinal tear)
- Larger retinal detachments (over 2 quadrants)
- Inferior retinal breaks
- Concomitant choroidal detachment
- Aphakia
- Inflammation (including excessive cryotherapy)
- Vitreous haemorrhage
- Lower socioeconomic status
- History of smoking
Pastor, J.C., et al., Proliferative vitreoretinopathy: risk factors and pathobiology. 2002. 21(1): p. 127-144.
Pastor, J.C., et al., Proliferative vitreoretinopathy: risk factors and pathobiology. 2002. 21(1): p. 127-144.
Cowley, M., et al., Clinical risk factors for proliferative vitreoretinopathy. 1989. 107(8): p. 1147-1151.
Girard, P., et al., Clinical risk factors for proliferative vitreoretinopathy after retinal detachment surgery. 1994. 14(5): p. 417-424.
Note
Paediatric patients are known to be at high risk of PVR, but age in adults has not been shown to correlate with risk of developing PVR. Patients with retinal detachment following trauma and in pigmented races are also likely to be at higher risk for PVR.
Patients with PVR retinal detachments require vitrectomy with epiretinal/subretinal membrane peeling ± relaxing retinectomy. In addition, lensectomy and scleral buckling should be considered. Factors that may influence this decision include:
1. Lensectomy via Phacoemulsification Surgery
Lensectomy should be especially considered in patients who are older or who have cataract. Removing the lens allows for better visualization and removal of the peripheral vitreous including anterior loop traction. Since an endotamponade will be used, insertion of an intraocular lens may be delayed as a secondary procedure. Aphakia allows for the most complete vitreous removal but invites the complications associated with aphakic oil if oil is the required tamponade. A peripheral iridectomy is required in aphakic eyes. It is often preferable to leave the capsule behind for future sulcus lens implantation, however remaining capsule can be a scaffold for anterior loop proliferation and for posterior synechiae. If the PVR is mainly posterior, implantation of a lens can be considered. Placement of a 3-piece lens may decrease the rate of capsular phimosis.
2. Scleral Buckle
If the breaks/PVR are anterior, the addition of an encircling scleral buckle provides extra support for these areas and the vitreous base.
If all three procedures are to be undertaken in the same operation, the usual sequence is:
- Scleral buckle
- Lensectomy
- Vitrectomy
- Retinectomy
Retinectomy in the setting of PVR should be considered when one or more of following are present:
- Focal contraction (star fold)
- Diffuse contraction
- Circumferential contraction
- Intrinsic retinal contraction
- Anterior retinal displacement
- Extensive fibrous periretinal proliferation
- Contraction and fibrosis of flap of giant retinal tear
Some important points to remember:
- Retinectomy should only be performed after all membranes have been removed
- A larger but more peripheral retinectomy is less functionally significant than a smaller posterior retinectomy
- Circumferential relaxing retinectomies are preferred to radial ones
- It is good to visualise the full extent of the retina before creation of the retinectomy. A wide-angle viewing system is best for this. Otherwise, scleral depression may need to be performed by the assistant
- Ensure adequate diathermy of the blood vessels and the area to be cut
- For maximum relaxation of traction, ensure that the retinectomy extends into the normal retina on both ends of the contracted area
Retinectomy Options:
- Wedge Retinectomy
- An anterior wedge retinectomy can be performed if the PVR is limited. A posterior retinectomy can be done in the setting of a single posterior starfold but in our experience most of these starfolds can be relaxed by peeling and posterior wedge retinectomies tend to have a low success rate
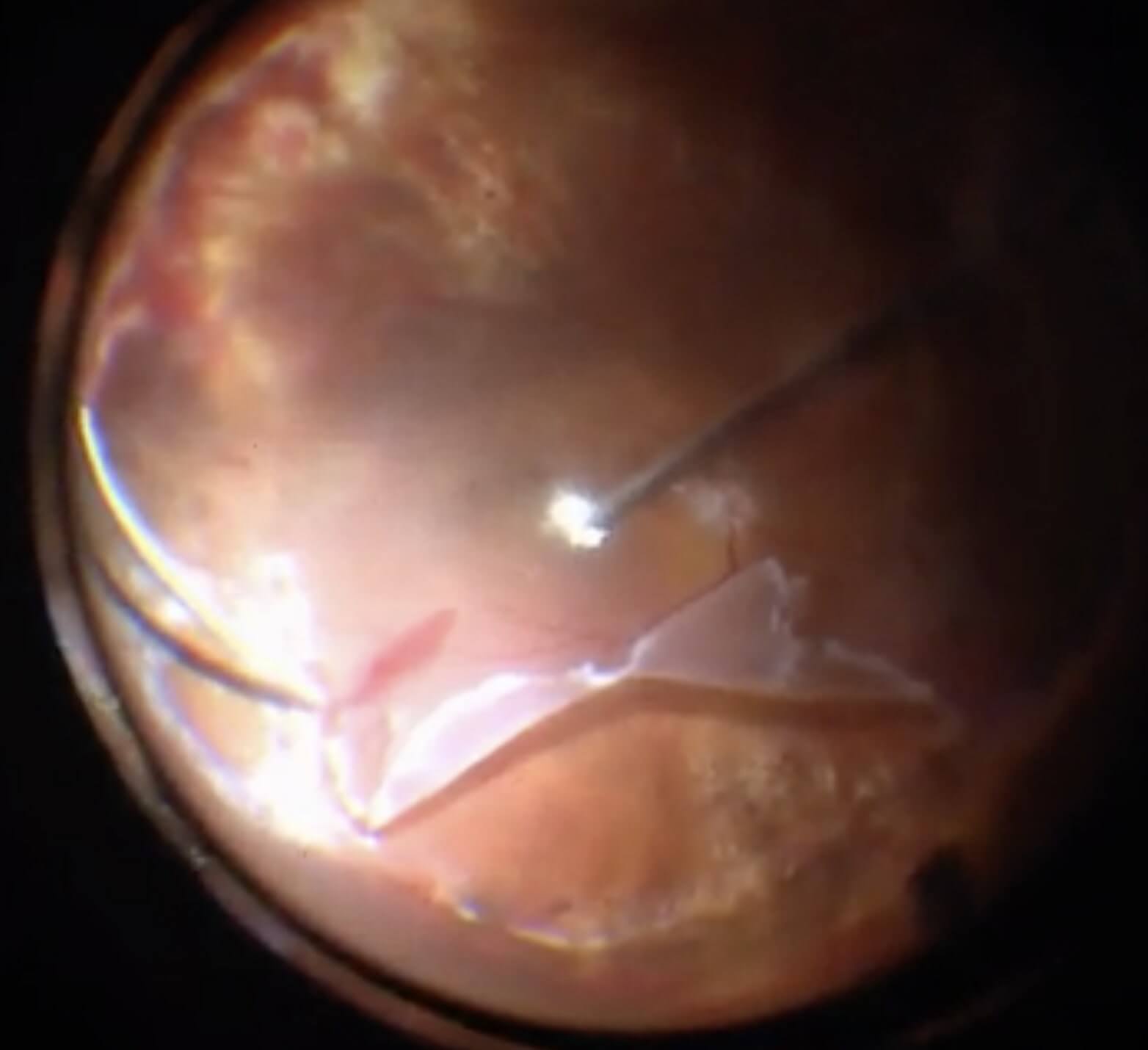
- Inferior 180-degree Retinectomy (Figure 8.3.1)
- Generally the preferred retinectomy if the contraction is more diffuse. The horns should be cleaned meticulously. Perfluorocarbon liquid (PFCL) can be used to stabilize the posterior pole while the retinectomy is performed. The retina anterior to the retinectomy should be excised. Consider laser versus cryotherapy for the horns. A buckle can be helpful to support the horns
- 270- or 360- degree Retinectomy
- Tend to be less stable (especially in 270 - degree) and visual outcomes tend to be poor. Try to avoid if possible. However, if needed to be performed, advisable to go for complete 360-degree circumferential retinectomy instead of 270 - degree. A scleral buckle is not necessary at this stage.
Endotamponade
The usual endotamponade is silicone oil or C3F8 gas. In the Silicone Study, C3F8 gas and silicone oil (1000 centistoke) were shown to be equivalent in terms of visual outcomes and re-attachment rates in patients with severe (at least grade C) PVR.[4] Long-term endotamponade may require a higher density of silicone oil (5000 centistoke) to prevent emulsification and glaucoma (Figure 8.3.2). “Heavy” silicone oils (e.g. Densiron® 68 and Densiron® Xtra) may be used for inferior PVR but should be removed within 3 months to avoid retinotoxicity. In severe cases of PVR, perfluoro-n-octane (PFO or “heavy liquid”) can be injected temporarily (1 - 2 weeks) to reattach the retina before being exchanged for silicone oil or C3F8 gas. It is important not to leave it longer than this since it is retinotoxic. Some surgeons will inject subtenon’s triamcinolone at the same time to mitigate the pro-inflammatory effects of PFO.
Vitrectomy With Silicone Oil or Sulfur Hexafluoride Gas in Eyes With Severe Proliferative Vitreoretinopathy: Results of a Randomized Clinical Trial: Silicone Study Report 1. JAMA Ophthalmology, 1992. 110(6): p. 770-779.
Various classification systems exist for grading PVR. The most commonly used classification by the Retina Society is shown below:[5]
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.