19.2 Retinal and Choroidal Biopsy for Inflammatory and Infectious Disease
Retino-choroidal biopsy has an important role in solving uveitic diagnostic dilemmas.[1] It is an invasive test with the potential for significant adverse effects and therefore should be reserved for cases in which less invasive samples such as vitreous biopsies have been inconclusive. The main indications for retino-choroidal biopsy are:[1,2,3]
- Progressive and sight-threatening retinitis or choroiditis which is worsening despite treatment
- To identify the causative organism or masquerade syndrome
- To differentiate between direct infection versus inflammation (e.g. sarcoidosis)
- Suspected neoplastic process
- To obtain a tissue diagnosis to guide chemo/radiotherapy
- When there is minimal vitreous involvement and predominantly retinal or subretinal pathology
- Following an inconclusive vitreous biopsy
- Immunocompromised patients (patterns of uveitis can be atypical in these patients)
- To differentiate between opportunistic infections and neoplastic causes
Johnston RL, Tufail A, Lightman S, Luthert PJ, Pavesio CE, Cooling RJ, Charteris D. Retinal and choroidal biopsies are helpful in unclear uveitis of suspected infectious or malignant origin. Ophthalmology 2004; 111:522-528.
Johnston RL, Tufail A, Lightman S, Luthert PJ, Pavesio CE, Cooling RJ, Charteris D. Retinal and choroidal biopsies are helpful in unclear uveitis of suspected infectious or malignant origin. Ophthalmology 2004; 111:522-528.
Charteris DG. Retinal biopsy. In: Hamilton AMP, Gregson RMC, Fish GE, eds. Text Atlas of the Retina. London: Butterworth-Heinemann Medical; 1998:107–11.
Jeroudi A, Yeh S. Diagnostic vitrectomy for infectious uveitis. Int Ophthalmol Clin. 2014;54:173-97.
- Good visual potential, where biopsy of another structure is feasible
- Monocular status (relative contraindication)
The two methods for obtaining a retinal and/or choroidal sample are endoretinal and trans-scleral. The approach depends on surgeon experience, but also depth of tissue involvement.
1. Endoretinal
This is the most utilised technique due to surgeon experience and overall risk/benefit profile.
Advantages:
- No large incisions into the eye
- Reduced risk of expulsive suprachoroidal haemorrhage
Disadvantages:
- Risk of haemorrhage and retinal detachment
- Small but potentially fatal risk of air / perfluorocarbon embolism[4,5]
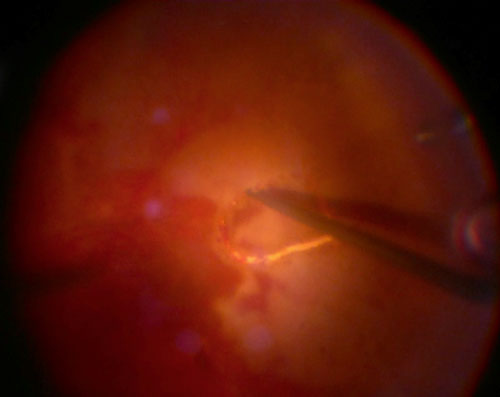
Technique:
Rice JC, Liebenberg L, Scholtz RP, Torr G. Fatal air embolism during endoresection of choroidal melanoma. Retin Cases Brief Rep. 2014;8:127-9.
Meraz Gutiérrez M, Camara Rodriguez E, Pando Cifuentes A, Ortiz-Ramirez G, Soberón Ventura V. Venous-air embolism during vitrectomy for endoresection of choroidal melanoma: Case report. Eur J Ophthalmol. 2021:112067212199510.
- The ideal biopsy site should be in an active lesion, preferably in the superior retina, and at the border of diseased and normal tissue
- Aim to take at least 2 x 2 mm size sample to maximise diagnostic yield
- A standard 3-port vitrectomy is carried out, using your preference of gauge. A pure undiluted vitreous sample and diluted vitreous washings from the cassette is sent off
- It is important to ensure complete elevation and removal of the posterior hyaloid from the area where the biopsy is taken from, otherwise this can become a focus for proliferative vitreoretinopathy (PVR) and increase the risk of postoperative retinal detachment. Triamcinolone assistance can be helpful to ensure complete hyaloid removal. (See Chapter 4 Posterior Vitreous Detachment Induction)
- Perform a broad area of diathermy or endolaser around the intended biopsy site. 810nm (diode) laser is preferred over 532nm, due to increased uptake in the choroid to aid haemostasis.[6] Ensure blood vessels are directly treated with diathermy
- Either unimanual or bimanual techniques can be used depending on surgeon preference
- Once a retinotomy is made, an initial subretinal biopsy can be performed using a flute cannula and this sample can be submitted separately
- The dissection of the retina or combined retina-choroid along the middle of the demarcated barrier can be performed using a combination of vertical and horizontal scissors (tip: raise the intraocular pressure to 80mmHg during this step and for a few minutes afterward to achieve hemostasis)
- A small pedicle is retained at the edge of the biopsy specimen to ensure that the sample remains in position while forceps are positioned ready to grasp it
- In order not to damage the sample, a port can either be removed and the sclerotomy enlarged, or a separate pars plana sclerotomy can be made to extricate the sample. One should not attempt to remove the tissue through a valved port. (tip: have an assistant clamp the infusion line during removal of the sample to prevent vitreous prolapse) An alternate method of removing the biopsy is by aspirating it into a blunt, large bore cannula connected to a syringe or by snagging it with a flex-loop
- Once removed, the sample should be inspected to ensure all components are present and have not been incarcerated in the wound. Pass the sample onto another team member to send to the lab
- Suture the sclerotomy and complete the remainder of the procedure for a standard vitrectomy
- The choice of tamponade depends on size, location and number of biopsy sites. For inferior biopsy sites, multiple biopsy sites or associated retinal necrosis, silicone oil tamponade may be preferred
- If there is no retinal detachment, avoid fluid-air exchange when there is a large area of exposed choroid close to vortex veins or if the biopsy is taken close to the posterior pole. A direct fluid-silicone oil exchange can be performed by passive extrusion of fluid with a backflush cannula during silicone oil injection
Cole CJ, Kwan AS, Laidlaw DA, Aylward GW. A new technique of combined retinal and choroidal biopsy. Br J Ophthalmol. 2008;92:1357-60.
2. Trans-Scleral
This approach is rarely used but may be preferred where a larger sample is required, or where the pathology is situated deep in the outer retina or choroid. Surgery should only be undertaken by surgeons experienced in the technique. Hypotensive general anaesthesia is used to reduce the risk of expulsive choroidal haemorrhage.
Advantages:
- A larger size biopsy can be taken
Disadvantages:
- Surgery more technically challenging
- Need for general anaesthetic
- Increased risk of complications
Technique:
- Localised peritomy is performed to expose the scleral bed and hemostasis is achieved with cautery (tip: to improve exposure, extraocular muscles may be slung with silk sutures or if the biopsy site is underneath an extraocular muscle it can be disinserted on pre-placed sutures)
- The biopsy site is localised with guidance from either transillumination or indirect ophthalmoscopy and marked using a skin marker with a 2-3 mm margin around the desired area
- Standard 3-port vitrectomy is performed along with vitreous samples
- Lamellar scleral dissection is performed using a 15-degree blade and crescent blade to create a 50% depth scleral flap hinged posteriorly
- Switch off or clamp the infusion line
- A smaller entry into the suprachoroidal space is made in the centre of the scleral bed and the choroid is exposed
- The choroid is resected with Vannas or similar scissors, either alone or in combination with the partial thickness scleral window. Care should be taken to avoid iatrogenic retinal trauma, unless one wishes to take a full thickness retinochoroidal biopsy. The risk of complications is lower if the retina is left intact
- The scleral flap is sutured using non-absorbable sutures e.g. 9-0 nylon, using as many sutures as required to achieve a water tight closure. Pre-placement of cardinal sutures facilitates rapid wound closure
- The infusion can now be switched back on
- Conjunctival closure can then be performed, with absorbable sutures or tissue glue. The latter has the advantage of aiding with sealing of the scleral flap
- The internal aspect of the biopsy is inspected and laser retinopexy applied to the fresh edge of the retina, if required
- Choice of tamponade depends on location of biopsy site and associated retinal pathology
As with all biopsy samples, it is imperative to discuss the requirements with the local laboratory which will be handling the sample prior to the surgical procedure. The sample is usually divided into smaller sections so that different laboratory tests can be carried out. Most laboratories request half of the specimen to be submitted fresh in phosphate buffered saline for microbiological testing and the other half to be sent in formalin. A third sample may also be submitted in RPMI for cytological analysis and flow cytometry.
Due to the precious nature of the sample, it is important to work with a pathology lab experienced in dealing with ocular tissues. Diagnostic yield is increased when tests are directed by clinical correlation so that appropriate stains and immunohistology are carried out. Table 1 lists the various tests which are often performed in the laboratory.
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.