Chapter 14
Vitreous Hemorrhage
Common causes of a vitreous hemorrhage include:
- Retinal tear, posterior vitreous detachment or retinal detachment
- Ischemic retinopathy secondary to proliferative diabetic retinopathy (DR), branch retinal vein occlusion (BRVO), sickle cell retinopathy, or ocular ischemic syndrome
- Breakthrough sub-retinal hemorrhage (e.g. neovascular age-related macular degeneration (AMD), retinal arteriolar macroaneurysm, Valsalva retinopathy, uveal tumour, Terson’s syndrome)
- Trauma
It is important to try to determine the cause of the vitreous hemorrhage pre-operatively by taking an adequate history (e.g. vascular risk factors, trauma, previous episodes, photopsias), examining both eyes and performing B-scan ultrasonography if fundus visualization is poor. In B-scan, it is important to perform a 360-degree dynamic scan to look for vitreous attachment, retinal detachment, presence of retina tears or elevation around the macula that could be suggestive of a breakthrough bleed from AMD. Fluorescein angiography may also be a useful adjunct if there is some visualization of the fundus.
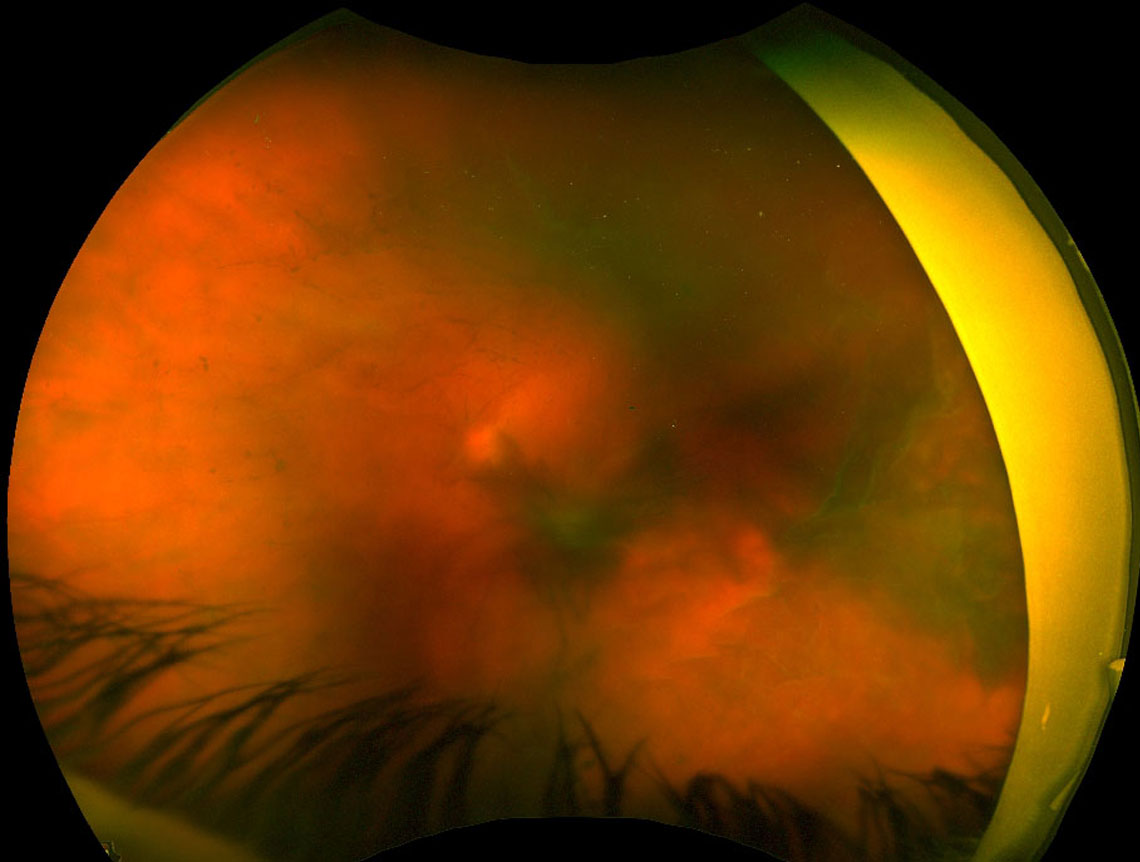
Management of vitreous hemorrhage is dependent on the cause and severity. Apart from vitrectomy to clear vitreous blood (Figure 14.1), the following adjuvant treatments may be required:
- Neovascularization secondary to retina ischemia: scatter laser photocoagulation in the area of capillary non-perfusion and/or anti-vascular endothelial growth factors (VEGF)
- Retinal tear: barrier laser retinopexy, endodiathermy to a bleeding bridging vessel
- Retinal detachment: vitrectomy for retinal re-attachment surgery
- Neovascular AMD: anti-VEGF, photodynamic therapy (if polypoidal choroidal vasculopathy)
- Retinal arteriolar macroaneurysms: focal laser, anti-VEGF
- Valsalva: YAG laser may be attempted instead of vitrectomy to disperse subhyaloid blood into the vitreous
Figure 14.1 Vitreous Hemorrhages
Figure 14.1 Vitreous Hemorrhages
- The infusion cannula should be visualised in the vitreous cavity prior to being turned on. Place the infusion cannula near the cutter port. This allows for earlier visualization of the infusion cannula, which is particularly important if its intravitreal position has been difficult to determine
- If intravitreal-visualization of the infusion cannula is not possible due to a dense vitreous hemorrhage, consider placing an anterior chamber infusion line first or consider a 6mm infusion in pseudophakic patients (the longer infusion has a higher risk of lens touch in phakic patients). If the infusion cannot be visualized the light pipe can be shone from outside the eye into the vitreous cavity for better visualization. Alternatively, the light pipe can be inserted into the cannula where the infusion is to be placed to confirm position prior to insertion of the infusion line
- If pre-operative B-scan ultrasonography has demonstrated a retinal detachment or suprachoroidal hemorrhage, position the sclerostomies appropriately to avoid sub- retinal and supra-choroidal entry whilst maximizing access to the pathology. Removal of the crystalline lens by pars plana lensectomy or by combined phacoemulsification may be needed to allow for more anterior trocar entry
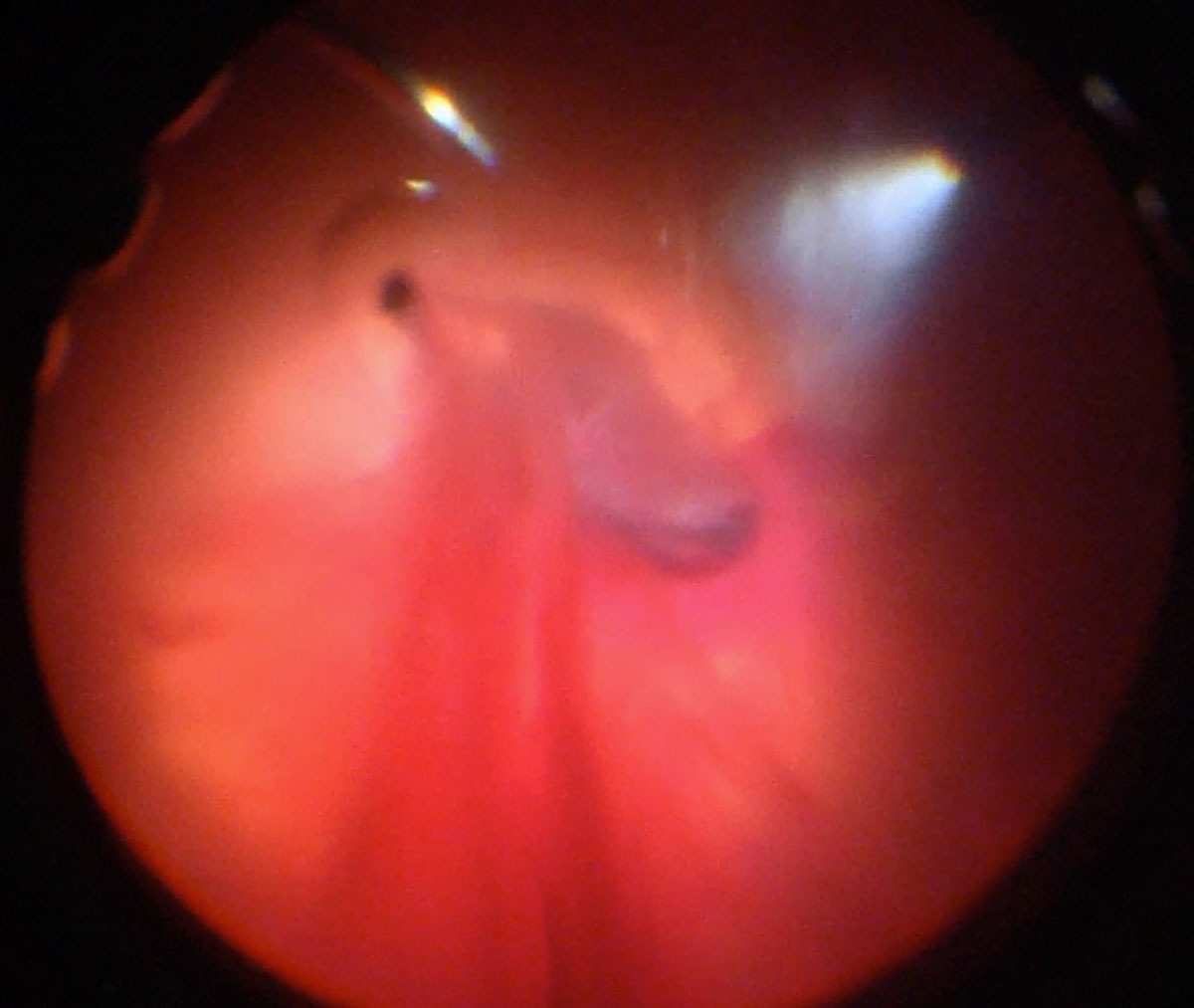
If there is significant anterior chamber hyphema that will obscure the view for vitrectomy, the anterior chamber may need to be cleared first. This is often most easily performed with the vitrector cutter through a paracentesis. Two paracenteses can be placed, one through which the infusion is introduced and the other through which the cutter is introduced to perform the washout.
(Figure 14.2 and Figure 14.3)
Remove vitreous (hemorrhage) from the core vitreous first. This allows for a safe vitrectomy in the event of an underlying retinal detachment. The view of the retina will slowly improve as hemorrhage is removed. It is important to ensure complete posterior vitreous detachment once the view is better. Consider starting the core in the superonasal position (a break is less detrimental in this position) or use the preoperative B scan as a guide for the safest area to start the vitrectomy.
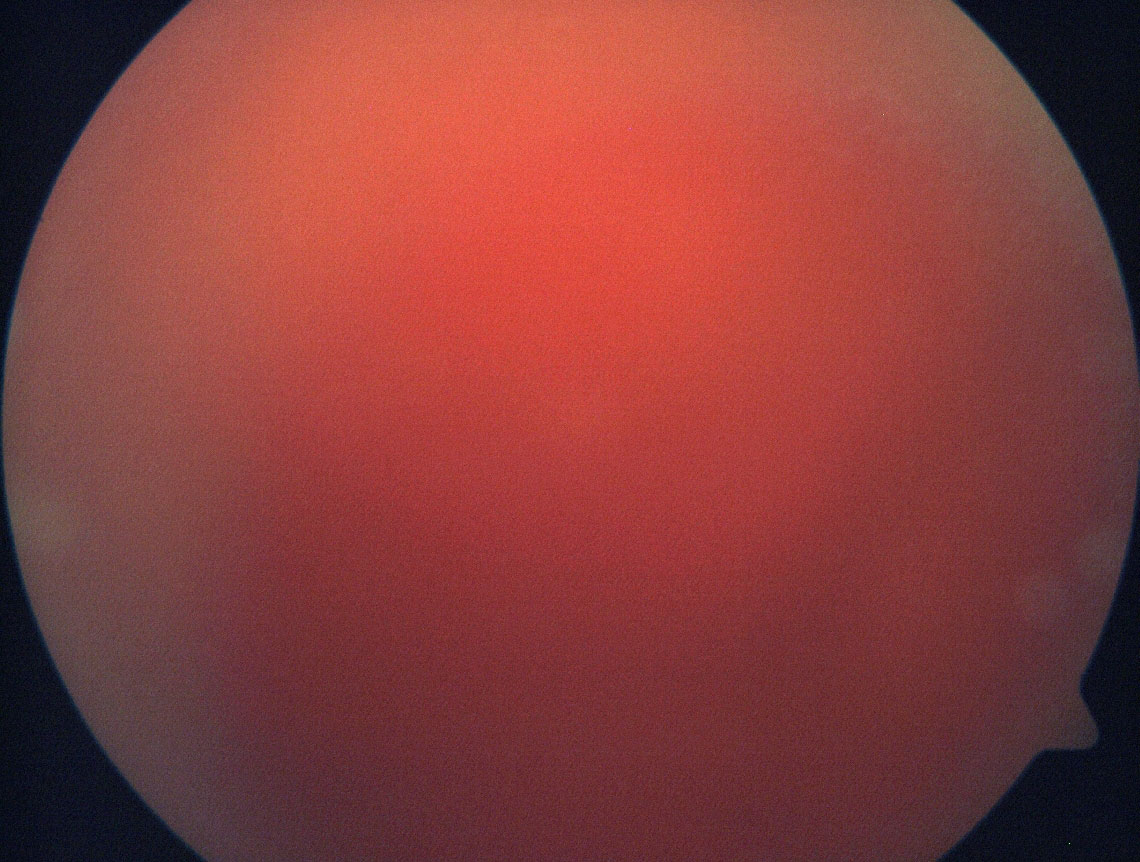
Figure 14.3 Dense Vitreous Hemorrhage
In cases of extremely dense clotted vitreous hemorrhage, great care must be taken to avoid inadvertently cutting detached retina. Vitrectomy should proceed from anterior to posterior, cutting only tissue that is well visualised. Retina can
identified by the presence of vessels.
As the view clears centrally, peripheral vitrectomy can be performed more safely. Remove clotted hemorrhage from the vitreous base, as this can leech post-operatively and cause recurrent vitreous hemorrhage. Scleral indentation of the (particularly inferior) periphery by the assistant (Figure 14.4) may be required to allow for a more complete vitrectomy, particularly in phakic patients. Beware of tears hidden in the vitreous base. Depressed shave should be done slowly with a low flow setting as sometimes the hemorrhage is khaki colored and visualization of the underlying retina is compromised, increasing the risk of an iatrogenic break. In phakic patients, vitreous just posterior to the lens should be cleared. Taking care not to traumatise the lens, blood on the posterior surface of the lens can be aspirated with the cutter, observing for a “trail” of blood moving towards the tip.
As the view clears, inspect for the cause of the vitreous hemorrhage. The management will depend on the underlying cause (see above):
- Retinal tear → Endolaser (or cryotherapy); Retinal detachment → repair
- Proliferative diabetic retinopathy → Pan-retinal photocoagulation
- Branch retinal vein occlusion → Sectoral retinal photocoagulation
Endodiathermy may be applied to any obvious source of bleeding (e.g. broken bridging vessel across a retinal tear).
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.