26 Lens Management
26.1 Phaco-Vitrectomy
26.2 Pars Plana Lensectomy
26.3 Intraocular Lens Explantation
26.4 Secondary Intraocular Lens Insertion Clinical Scenarios & Clinical Decision Making
26.5 Sulcus Intraocular Lens
26.6 Anterior Chamber Intraocular Lens
26.7 Iris Fixated Intraocular Lenses
26.8.1 Scleral Sutured Intraocular Lens – Traditional 2 Point Fixation
26.8.2 Scleral Sutured Posterior Chamber Intraocular Lens 4 Point Fixation
26.8.3 Scleral Sutured Posterior Chamber Intraocular Lens – “Hoffman” Corneoscleral Pockets
26.8.4 Alternate Technique to Rescue a Dislocated IOL – Triangular Scleral Flap, Sutured IOL Technique
26.8.5 Suturing Without Exchanging the Intraocular Lens
26.9 Sutureless Scleral Fixation of an Intraocular Lens
26.8.5 Suturing Without Exchanging the Intraocular Lens
If the subluxed/dislocated IOL is three-piece or a rigid one-piece, it may be suitable for scleral fixation. This has the advantage of avoiding a large wound to exchange the IOL. The technique is more difficult, however.
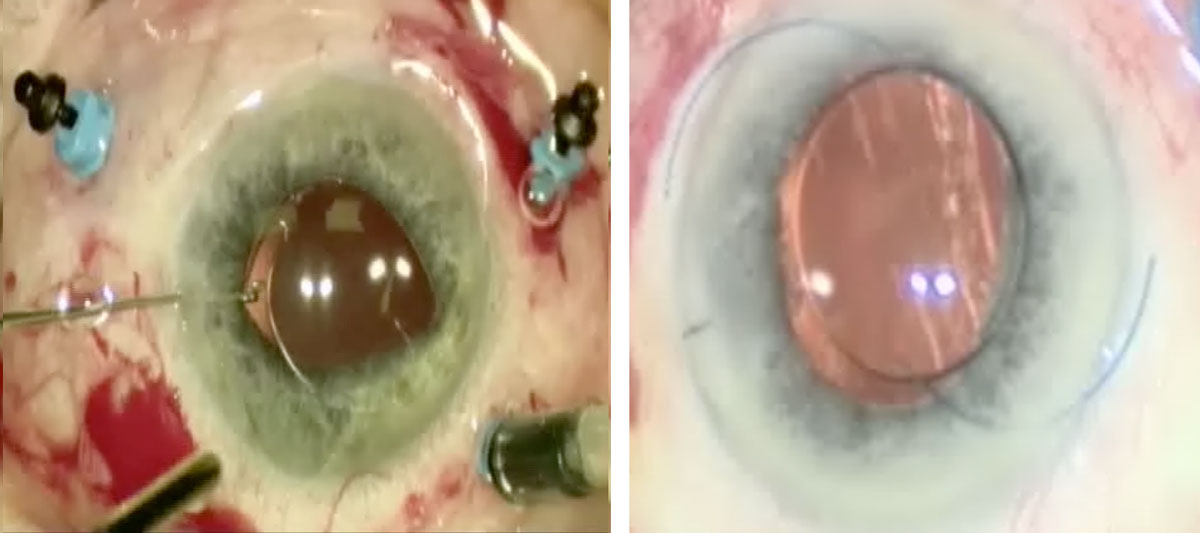
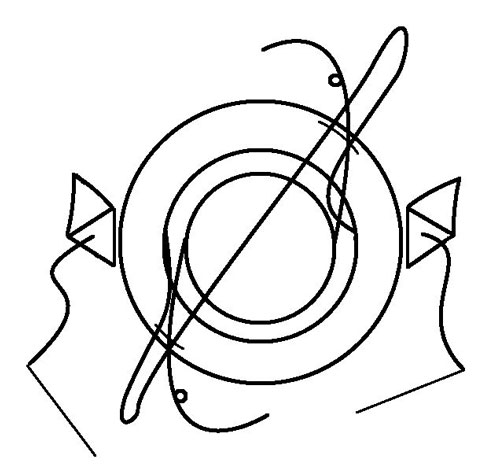
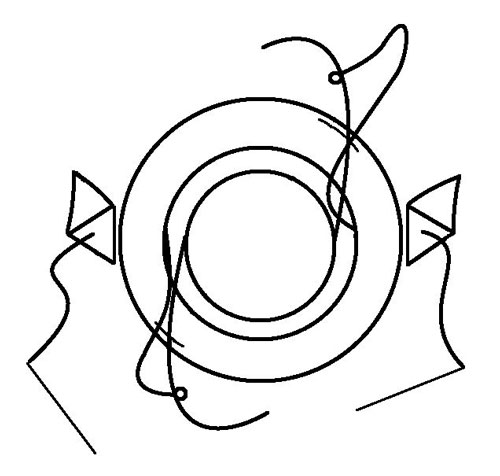
1. Three-piece IOL with Flexible Haptics (Figure 26.8.5.1)
First bring the IOL into the anterior chamber. Fashion paracenteses near them (180 apart) and externalise both haptics through these. Fashion scleral flaps (or grooves) perpendicular to the paracenteses. Pass a 10-0 Prolene* suture across the eye (behind the iris) underneath the scleral flaps or through the grooves. Externalise a loop of this suture through each paracentesis with a Sinskey or Kuglen hook. Cut each loop and suture the cut ends to the haptics. Internalise the IOL and tie the Prolene* sutures underneath the scleral flaps (or within the grooves).
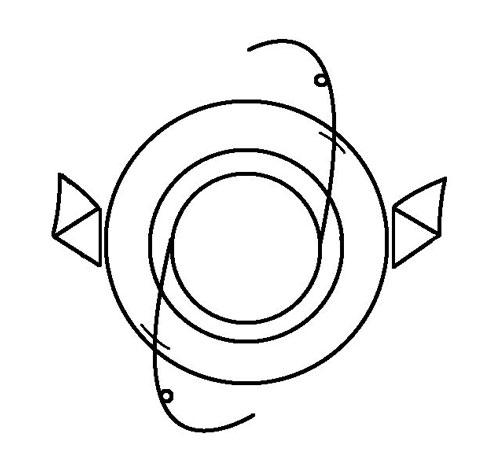
Figure 26.8.5.1 Suturing a Dislocated Intraocular Lens
A: A three-piece IOL may be suitable for scleral fixation
B: The IOL haptics are externalised through paracenteses 180º apart
C: The 10-0 Prolene* suture is passed across the eye. Loops of this suture from within the pupil are externalised through each of the paracenteses
D: One of the suture loops is cut and the cut ends sutured to the islets of the haptics. The ends of the 10-0 Prolene* suture (with needles) are sutured underneath the sclera flaps (or grooves)
C
D
Figure 26.8.5.1 Suturing a Dislocated Intraocular Lens
A: A three-piece IOL may be suitable for scleral fixation
B: The IOL haptics are externalised through paracenteses 180º apart
C: The 10-0 Prolene* suture is passed across the eye. Loops of this suture from within the pupil are externalised through each of the paracenteses
D: One of the suture loops is cut and the cut ends sutured to the islets of the haptics. The ends of the 10-0 Prolene* suture (with needles) are sutured underneath the sclera flaps (or grooves)
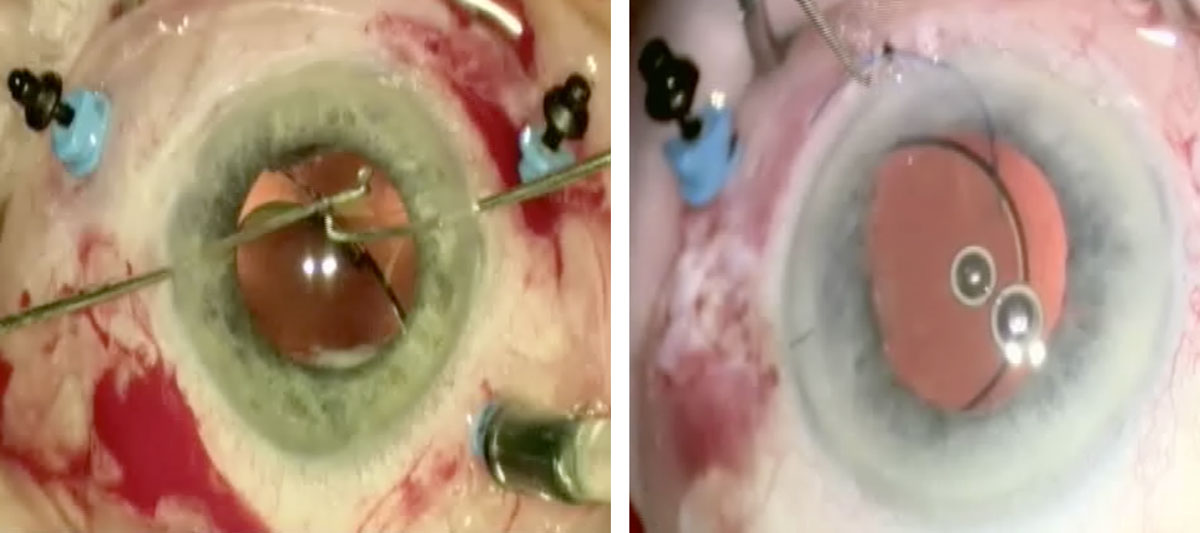
Figure 26.8.5.2 Manipulating the IOL into the Anterior Chamber
Certain dislocated IOLs may be suitable for scleral fixation without exchange of the IOL. The IOL should be manipulated into the anterior chamber. The vitrectomy cutter, light pipe, Sinskey hook, Kuglen hook or microforceps can be used to perform this step. It is often easiest to have a limbal paracentesis through which the instrument is inserted to bring the IOL from the posterior to the anterior chamber.
2. Rigid One-piece IOL
In this scenario it is difficult to externalise both haptics simultaneously without traumatising the IOL. One haptic can be externalised, sutured and internalised at a time prior to suturing to sclera (as above). Alternatively, use the following technique to “loop” the haptic:
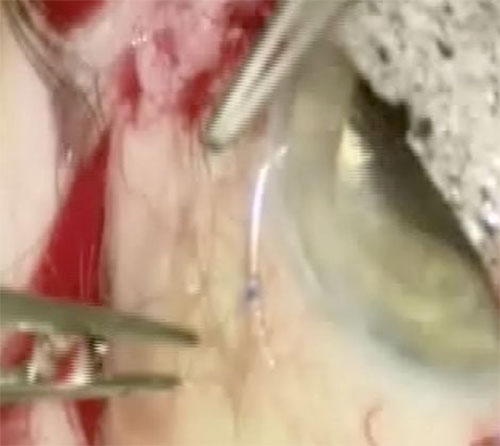
If the IOL is only subluxed (not dislocated), it may not be necessary to bring it into the anterior chamber. If the IOL is fully dislocated, bring the haptic that is opposite to the one being sutured into the anterior chamber (in front of the iris) for stabilisation. It is easiest to use a double-armed 10-0 Prolene* suture with straight needles. Fashion scleral flaps or grooves as above. Create a limbal paracentesis approximately 90 away from this with a keratome blade. Pass the Prolene* needle through the paracentesis underneath the haptic (lying behind the iris) and out underneath the scleral flap (or through a groove). Attempts to pass a needle through a haptic islet within the eye usually prove unsuccessful. A 27-gauge needle can be passed underneath the scleral flap (or through a groove) ab externo to assist with externalisation of the Prolene* needle. Ensure that no corneal tissue is caught by the Prolene* needle as it passes through the paracentesis. Repeat with the straight needle at the other end of the Prolene* suture, but this time pass it over the haptic. Cut the needles off the two ends of the Prolene* suture, and suture these together (underneath the scleral flap or within a groove). Repeat the process for the opposite haptic, which can now be placed posterior to the iris.
Alternatively (or if the suture is single armed), pass it underneath the scleral flap (or groove) first, under the haptic, out the paracentesis, back in the paracentesis, over the haptic and back out underneath the scleral flap (or groove). (Figure 26.8.5.5).
Alternatively, thread a single-armed 10-0 Prolene* suture through a 27-gauge needle and pull the suture through. Use the 27-gauge needle to enter the eye underneath the scleral flap (or through a groove) ab externo. Using a Kuglen hook through an opposite paracentesis, manipulate the IOL haptic such that the loop of 10-0 Prolene* suture emanating from the 27-gauge needle loops around the end of the haptic. Remove the 27 gauge needle, and tie the ends of the ends of the 10-0 Prolene* suture underneath the scleral flap or within a groove. (Figure 26.8.5.6).
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.