18 Symptomatic Vitreous Opacities
18.2 YAG Laser Vitreolysis
Yttrium aluminum garnet (YAG) laser vitreolysis (YLV) has recently gained prominence for the treatment of symptomatic vitreous opacities (floaters) and may be considered as an alternative to pars plana vitrectomy.
Patient Selection
YAG laser vitreolysis has previously been compared to sham and been found to be safe and efficacious.[1] Pre-treatment examination should be centered on the patient history, in particular impact on activities of daily living (ADL). Furthermore, active inflammation (vitritis) and active retinal pathology (posterior uveitis) should be ruled out before considering treatment. In general, eyes with a recent posterior vitreous detachment should be monitored for at least 6-12 months to allow for neuroadaptation prior to considering YLV.[2] In eyes with pre-existing lattice degeneration or retinal holes, laser retinopexy should be considered prior to YVL. Strong lenticular astigmatism can be a challenge for the procedure as it may make focusing the laser difficult. The ideal candidates for YLV are as follows:
Shah CP, Heier JS. YAG Laser Vitreolysis vs Sham YAG Vitreolysis for Symptomatic Vitreous Floaters. JAMA Ophthalmol. 2017;135(9):918.
Katsanos A, Tsaldari N, Gorgoli K, Lalos F, Stefaniotou M, Asproudis I. Safety and Efficacy of YAG Laser Vitreolysis for the Treatment of Vitreous Floaters : An Overview. Adv Ther. 2020.
- Symptomatic vitreous opacities impairing ADLs
- Single vitreous floater
- Mid-vitreous location (Figures 18.2.1)
- Weiss ring or degenerated Weiss ring (a patient without a PVD may present greater risk with the procedure)
- Pseudophakic status
- Clearly visible opacity which is accessible with laser contact lens
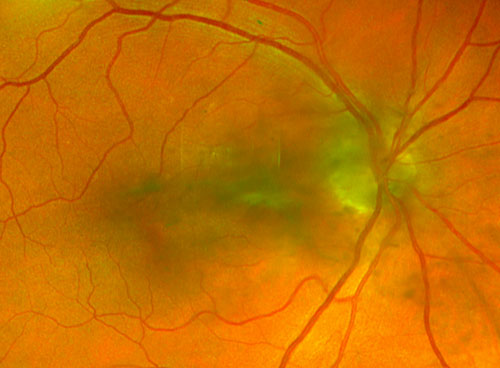
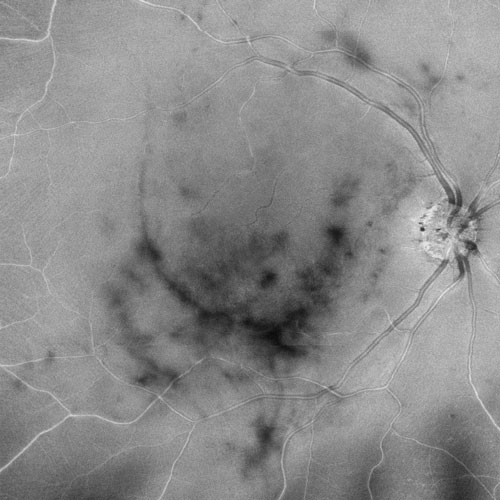
Figure 18.2.2
Enface swept source OCT (Zeiss Plex Elite, Carl Zess Meditec, Germany) of vitreous opacity of patient in Figure 18.2.1, demonstrating location over macula.
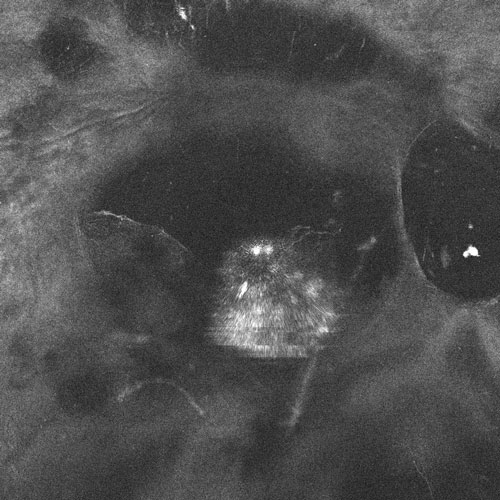
Figure 18.2.3
Enface swept source vitreous OCT (Zeiss Plex Elite, Carl Zeiss Meditec, Germany) demonstrating a hyperreflective diffuse opacity in the vitreous cavity of the patient depicted in Figure 18.2.1.
A. Pre-operative Imaging
- SLO-UWF imaging can be effective in confirming the presence of the vitreous opacity pre-treatment and correlating to the patient’s description / symptoms (Figure 18.2.1)
- Enface Optical coherence tomography (OCT) can be used to confirm the impact of visual impairment (shadowing over retinal tissue) (Figure 18.2.2)
- Dynamic OCT can also be performed to detect movement of the vitreous opacity in vivo within the vitreous and its resultant real-time shadowing over the macula (Video 18.2.1)
- Enface Vitreous OCT is an evolving modality whereby multiple opacities can be visualized within the vitreous to visualize the opacity and their relationship to retinal structures (Figure 18.2.3)
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.