16.4 Myopic Traction Maculopathy – Vitrectomy
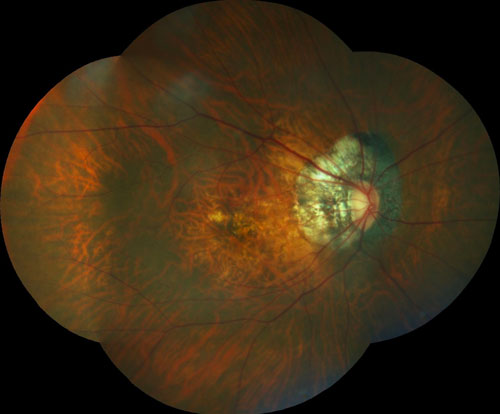
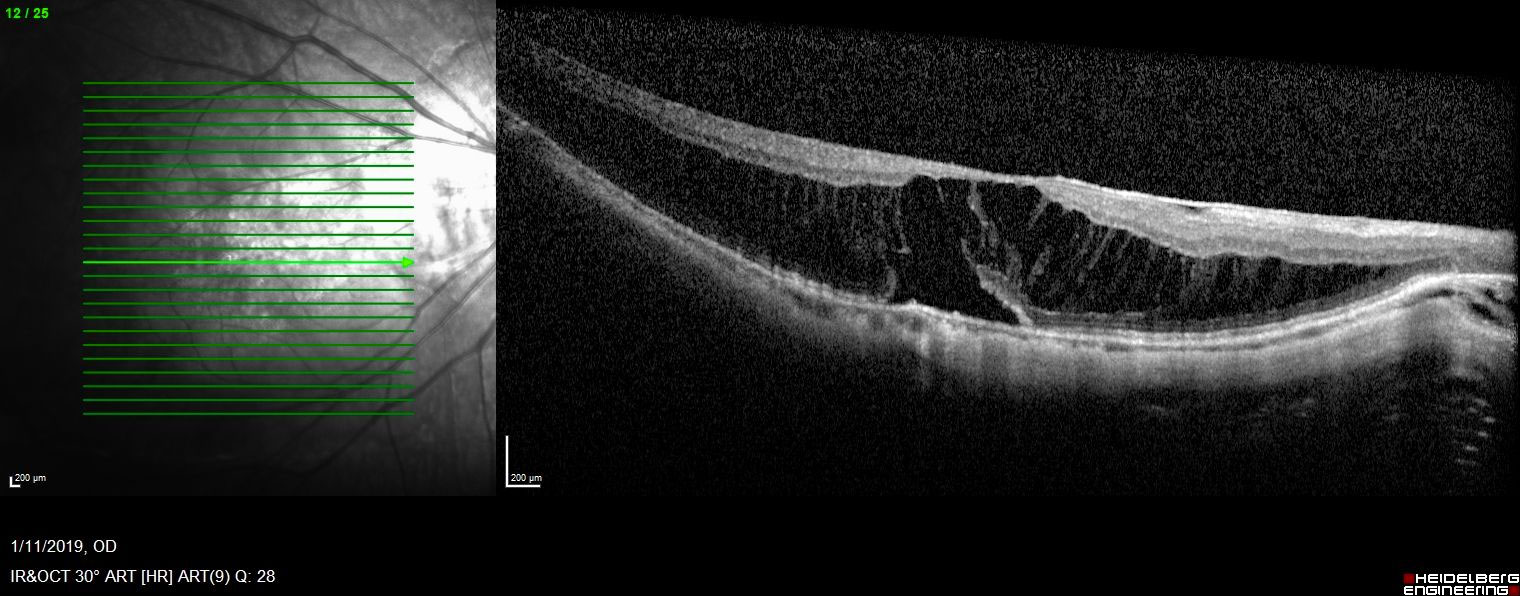
Myopic traction maculopathy comprises a series of entities including macular retinoschisis or foveoschisis, foveal detachment as well as FTMH.[1,2,3] Pathologies involve, among others, syneresis and vitreoschisis, an abnormal vitreoretinal interface, elongated axial length, posterior staphyloma, and reduced retinal pigment epithelial (RPE) function (Figure 16.4.1 and Figure 16.4.2). Surgical options for management include macular buckle as well as pars plana vitrectomy. In the following, management by PPV is discussed.
Wakazono T, Yamashiro K, Miyake M, et al. Association between Eye Shape and Myopic Traction Maculopathy in High Myopia. Ophthalmology 2016;123(4):919-21.
Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol 2007;125(6):767-72.
Baba T, Ohno-Matsui K, Futagami S, et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol 2003;135(3):338-42.
Some general considerations apply when operating on a long eye. First, local anaesthesia by retrobulbar / peribulbar block may best be avoided due to the risk of globe perforation in the presence of a posterior staphyloma. Secondly, standard vitrectomy instruments may be too short to reach the back of the eye in extreme cases. Strategies to circumvent this problem are use of special, longer instruments.[1] 20-gauge instruments are longer than MIVIS instrumentation, but rarely used today (note 23g instrumentation which is more available is slightly longer than 25 or 27g instrumentation).[2] Removing the cannulae and entering the eye directly through the sclerostomy provides a few millimeters additional reach. It is also possible to indent the sclera using the instrument hub.
Wakazono T, Yamashiro K, Miyake M, et al. Association between Eye Shape and Myopic Traction Maculopathy in High Myopia. Ophthalmology 2016;123(4):919-21.
Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol 2007;125(6):767-72.
The best indication for surgery in macular retinoschisis is presence of a foveal detachment in the outer retinal layers. The disease can progress to a myopic full-thickness macular hole (FTMH). Aggressive ILM peeling also risks an idiopathic FTMH developing after surgery.
1. Elevation of the Posterior Hyaloid (Posterior Vitreous Detachment (PVD)
High myopia tends to have vitreoschisis rather than a total PVD. Before ILM peeling, the posterior hyaloid membrane should be entirely removed, by the vitreous cutter, soft tip extrusion or forceps. Triamcinolone acetonide can be used to visualize the vitreous (Figures 16.4.3).
All rights reserved. No part of this publication which includes all images and diagrams may be reproduced, distributed, or transmitted in any form or by any means, including photocopying, recording, or other electronic or mechanical methods, without the prior written permission of the authors, except in the case of brief quotations embodied in critical reviews and certain other noncommercial uses permitted by copyright law.
Westmead Eye Manual
This invaluable open-source textbook for eye care professionals summarises the steps ophthalmologists need to perform when examining a patient.